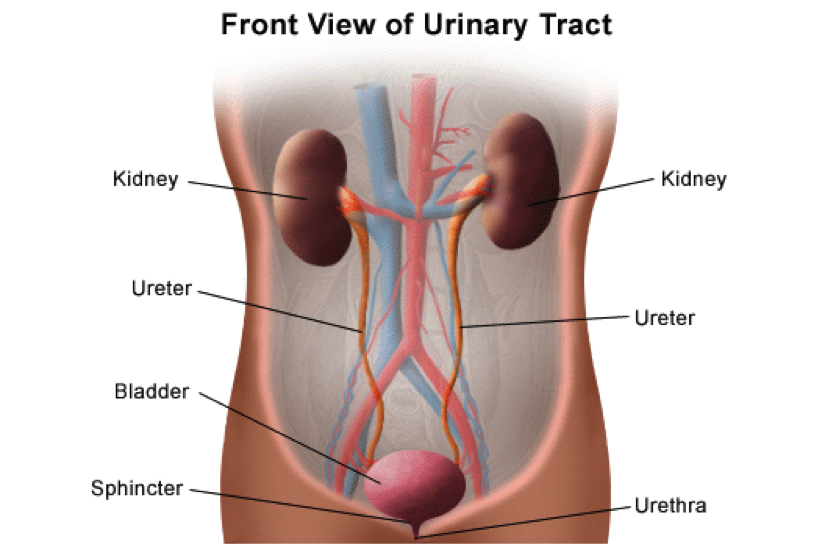
THE URINARY SYSTEM – BLADDER CARE AND MANAGEMENT
The 5 parts of the urinary system work to excrete waste (urine) and keep the chemicals and water in your body balanced. The kidneys are bean-shaped organs about the size of a fist. Urine is made in the kidneys and travels down two thin tubes called Ureters to the bladder. The bladder is a muscular organ shaped like a balloon. The urine is stored in the bladder until it gets full. The sphincter muscles close tightly like a rubber band around the opening of the bladder to help keep urine in the bladder. As the bladder fills with urine, the sensation to urinate becomes stronger. At the point when the bladder reaches its limits, nerves from the bladder send a message to the brain that the bladder is full. To urinate, the brain signals the sphincter muscles to relax. At the same time, the brain signals the bladder muscles to tighten, squeezing urine out of the bladder. When all the signals work normally, the urine exits the bladder through the urethra.
AFTER SPINAL CORD INJURY
After a spinal cord injury (SCI), 3 parts of the urinary system continue to function normally. The kidneys continue to make urine, and urine continues to flow through the ureters and urethra. These functions are involuntary responses, meaning they act without the need for the brain to tell them to. The bladder and sphincter are voluntary muscles that need the brain to coordinate the emptying of the bladder. Such messages are normally sent through nerves near the end of the spinal cord (the sacral level of the spine). However, those messages may no longer travel through the spinal cord after an injury. This means that individuals with SCI may not feel the “urge” to urinate when their bladder is full. They also may not have voluntary control of their bladder and sphincter muscles. The bladder is usually affected in one of two ways:
- Spastic (Reflex) bladder is when your bladder fills with urine and a reflex automatically triggers the bladder to empty. One major problem with a spastic bladder is that an individual does not know when, or if, the bladder will empty
- Flaccid (Non-reflex) bladder is when the reflexes of the bladder muscles are sluggish or absent. If you do not feel when the bladder is full, it can become over-distended, or stretched. The urine can back up through the ureters into the kidneys. Stretching also affects the muscle tone of the bladder.
The sphincter muscles may also be affected after injury. Dyssynergia occurs when the sphincter muscles do not relax when the bladder contracts. The urine cannot flow through the urethra. This results in the urine backing up into the kidneys. This is called “reflux” action. The bladder also may not empty completely. Treatments include medications or surgery to open the sphincter.
BLADDER MANAGEMENT METHODS
Although individuals with SCI may lack the sensation, or “urge” to urinate, the bladder will still need to be emptied. If not, the bladder muscles stretch as the bladder fills, and urine backs up into the ureters and kidneys. This is called Reflux. Reflux damages the bladder, ureters and kidneys. Failure to empty the bladder to relieve pressure can result in serious health problems, even death.
Every individual is different, so it is important that the treating doctor work together with the injured individual to choose a bladder management method that is convenient to empty the bladder. Keep in mind that an effective management program helps to avoid bladder accidents and prevent complications such as infections.
Considerations for designing a bladder management program include the individual’s mobility, finger dexterity, daily lifestyle, loss of normal urinary system function, and their susceptibility to infections. If the individual suffers from a Spastic (Reflex) bladder, the bladder management method will likely be an intermittent catheterization program (ICP), indwelling catheter (Foley or Suprapubic), or a male external condom catheter. ICP is usually the method of choice for individuals to empty a flaccid bladder.
URINARY SYSTEM CARE
An individual with spinal cord injury is at risk for a number of potential urinary system complications. Proper bladder care is the best way to prevent problems and maintain short- and long-term health. Following a self-care checklist is a great way to help prevent potential complications.
Drinking the proper amount of water is one of the most important factors for bladder care. A very important consideration in determining the proper bladder management method is to ascertain how much water the individual typically needs on a daily basis.
Indwelling Catheter – it is recommended that each day the individual drinks about 15 (8oz) glasses of water, which is about 3 quarts.
Condom and Intermittent Catheterization (ICP) – it is recommended that the individual drinks between 8 to 10 (8oz) glasses of liquid per day, which is about 2 quarts. There may be circumstances when drinking more water than recommended is necessary. For example, an individual may need to drink more water if he/she also drinks beverages that contain sugar, caffeine or alcohol. More water is necessary because these drinks cause individuals to urinate more often, which means the body absorbs less water. There may also be circumstances when individuals need to drink less than the recommended amount of water. Less water is necessary if you have another health condition such as congenital heart failure. Of course, individuals should always consult with their doctor if questions arise.
Although a regularly scheduled ICP is preferred, there is really no “recommended” time between intermittent catheterization. If an individual drinks the recommended amounts of water each day, catheterization may only be necessary every 3 or 4 hours. Catheterization will be necessary more often if an individual drinks more liquids or if his/her bladder capacity is less than normal (13-16 ounces). Generally speaking, it is ideal to drink most of the fluids between breakfast (6am) and dinner (6pm). This time frame allows the individual to get his/her daily intake of liquids and empty his/her bladder just before going to bed (10pm). Because your body’s organs usually slow while sleeping, individuals can usually sleep through the night without the need to catheterize before the next morning. If the 6 to 6 time frame does not suit an individual’s lifestyle, adjust the time frame to fit his/her schedule.
Using a “sterile” ICP technique can help individuals stay as germ-free as possible. Sterile ICP kits are one-time use catheters. These ICP kits are also known as “touch free” or “touch less,” which refers to the ability to catheterize oneself without the need to touch the insertion tube. Due to a revised reimbursement policy covering the use of intermittent catheters, most people who have insurance can now get a maximum of 200 intermittent catheters per month instead of the 4 catheters per month under the previous policy. The change should allow most users to obtain the closed, sterile ICP kits. Ask your health care provider or contact your insurance provider for more information. Although a closed, sterile system is preferred for ICP, many individuals with SCI still use a “clean” catheterization technique.