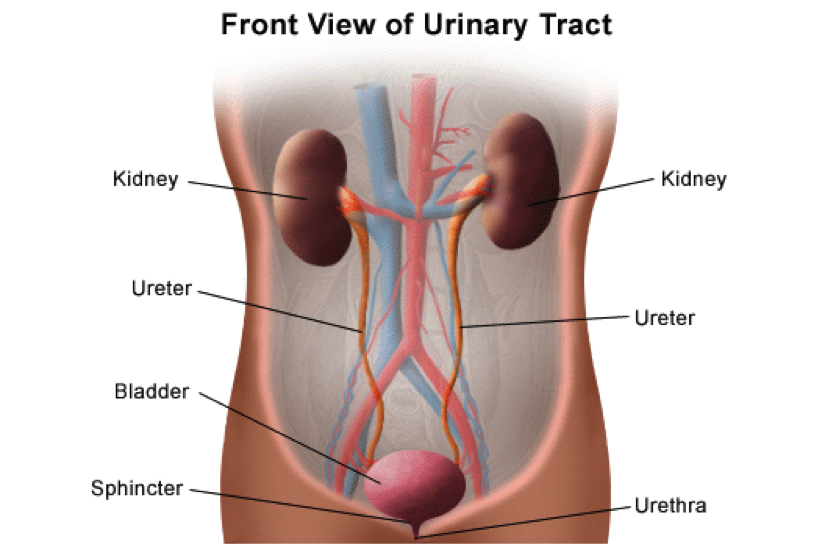
THE URINARY SYSTEM – BLADDER CARE AND MANAGEMENT
The 5 parts of the urinary system work to excrete waste (urine) and keep the chemicals and water in your body balanced. The kidneys are bean-shaped organs about the size of a fist. Urine is made in the kidneys and travels down two thin tubes called Ureters to the bladder. The bladder is a muscular organ shaped like a balloon. The urine is stored in the bladder until it gets full. The sphincter muscles close tightly like a rubber band around the opening of the bladder to help keep urine in the bladder. As the bladder fills with urine, the sensation to urinate becomes stronger. At the point when the bladder reaches its limits, nerves from the bladder send a message to the brain that the bladder is full. To urinate, the brain signals the sphincter muscles to relax. At the same time, the brain signals the bladder muscles to tighten, squeezing urine out of the bladder. When all the signals work normally, the urine exits the bladder through the urethra.
AFTER SPINAL CORD INJURY
After a spinal cord injury (SCI), 3 parts of the urinary system continue to function normally. The kidneys continue to make urine, and urine continues to flow through the ureters and urethra. These functions are involuntary responses, meaning they act without the need for the brain to tell them to. The bladder and sphincter are voluntary muscles that need the brain to coordinate the emptying of the bladder. Such messages are normally sent through nerves near the end of the spinal cord (the sacral level of the spine). However, those messages may no longer travel through the spinal cord after an injury. This means that individuals with SCI may not feel the “urge” to urinate when their bladder is full. They also may not have voluntary control of their bladder and sphincter muscles. The bladder is usually affected in one of two ways:
- Spastic (Reflex) bladder is when your bladder fills with urine and a reflex automatically triggers the bladder to empty. One major problem with a spastic bladder is that an individual does not know when, or if, the bladder will empty
- Flaccid (Non-reflex) bladder is when the reflexes of the bladder muscles are sluggish or absent. If you do not feel when the bladder is full, it can become over-distended, or stretched. The urine can back up through the ureters into the kidneys. Stretching also affects the muscle tone of the bladder.
The sphincter muscles may also be affected after injury. Dyssynergia occurs when the sphincter muscles do not relax when the bladder contracts. The urine cannot flow through the urethra. This results in the urine backing up into the kidneys. This is called “reflux” action. The bladder also may not empty completely. Treatments include medications or surgery to open the sphincter.
BLADDER MANAGEMENT METHODS
Although individuals with SCI may lack the sensation, or “urge” to urinate, the bladder will still need to be emptied. If not, the bladder muscles stretch as the bladder fills, and urine backs up into the ureters and kidneys. This is called Reflux. Reflux damages the bladder, ureters and kidneys. Failure to empty the bladder to relieve pressure can result in serious health problems, even death.
Every individual is different, so it is important that the treating doctor work together with the injured individual to choose a bladder management method that is convenient to empty the bladder. Keep in mind that an effective management program helps to avoid bladder accidents and prevent complications such as infections.
Considerations for designing a bladder management program include the individual’s mobility, finger dexterity, daily lifestyle, loss of normal urinary system function, and their susceptibility to infections. If the individual suffers from a Spastic (Reflex) bladder, the bladder management method will likely be an intermittent catheterization program (ICP), indwelling catheter (Foley or Suprapubic), or a male external condom catheter. ICP is usually the method of choice for individuals to empty a flaccid bladder.
URINARY SYSTEM CARE
An individual with spinal cord injury is at risk for a number of potential urinary system complications. Proper bladder care is the best way to prevent problems and maintain short- and long-term health. Following a self-care checklist is a great way to help prevent potential complications.
Drinking the proper amount of water is one of the most important factors for bladder care. A very important consideration in determining the proper bladder management method is to ascertain how much water the individual typically needs on a daily basis.
Indwelling Catheter – it is recommended that each day the individual drinks about 15 (8oz) glasses of water, which is about 3 quarts.
Condom and Intermittent Catheterization (ICP) – it is recommended that the individual drinks between 8 to 10 (8oz) glasses of liquid per day, which is about 2 quarts. There may be circumstances when drinking more water than recommended is necessary. For example, an individual may need to drink more water if he/she also drinks beverages that contain sugar, caffeine or alcohol. More water is necessary because these drinks cause individuals to urinate more often, which means the body absorbs less water. There may also be circumstances when individuals need to drink less than the recommended amount of water. Less water is necessary if you have another health condition such as congenital heart failure. Of course, individuals should always consult with their doctor if questions arise.
Although a regularly scheduled ICP is preferred, there is really no “recommended” time between intermittent catheterization. If an individual drinks the recommended amounts of water each day, catheterization may only be necessary every 3 or 4 hours. Catheterization will be necessary more often if an individual drinks more liquids or if his/her bladder capacity is less than normal (13-16 ounces). Generally speaking, it is ideal to drink most of the fluids between breakfast (6am) and dinner (6pm). This time frame allows the individual to get his/her daily intake of liquids and empty his/her bladder just before going to bed (10pm). Because your body’s organs usually slow while sleeping, individuals can usually sleep through the night without the need to catheterize before the next morning. If the 6 to 6 time frame does not suit an individual’s lifestyle, adjust the time frame to fit his/her schedule.
Using a “sterile” ICP technique can help individuals stay as germ-free as possible. Sterile ICP kits are one-time use catheters. These ICP kits are also known as “touch free” or “touch less,” which refers to the ability to catheterize oneself without the need to touch the insertion tube. Due to a revised reimbursement policy covering the use of intermittent catheters, most people who have insurance can now get a maximum of 200 intermittent catheters per month instead of the 4 catheters per month under previous policy. The change should allow most users to obtain the closed, sterile ICP kits. Ask your health care provider or contact your insurance provider for more information. Although a closed, sterile system is preferred for ICP, many individuals with SCI still use a “clean” catheterization technique.
STEP BY STEP ICP PROCESS FOR MEN:
Step 1 Assemble all equipment: catheter, lubricant, drainage receptacle (container).
Step 2 Wash your hands thoroughly with soap and water and clean the penis and opening of the urethra.
Step 3 Lubricate the catheter.
Step 4 Hold the penis on the sides, perpendicular to the body.
Step 5 Begin to gently insert and advance the catheter.
Step 6 You will meet resistance when you reach the level of the prostate. Try to relax by deep breathing, and continue to advance the catheter.
Step 7 Once the urine flow starts, continue to advance the catheter another 1 inch. Hold it in place until the urine flow stops and the bladder is empty.
Step 8 Remove the catheter in small steps to make sure the entire bladder empties.
Step 9 Wash the catheter with soap and water. If the catheter is disposable, discard it right away. If it is reusable, rinse the catheter completely and dry the outside. Store the catheter in a clean, dry location.
STEP BY STEP ICP PROCESS FOR WOMEN:
Step 1 Assemble all equipment: catheter, lubricant, drainage receptacle.
Step 2 Wash your hands thoroughly with soap and water and clean the vulva and opening of the urethra.
Step 3 Lubricate the catheter.
Step 4 Locate the urethral opening. The opening is located below the clitoris and above the vagina.
Step 5 Spread the lips of the vagina (labia) with the second and fourth finger, while using the middle finger to feel for the opening.
Step 6 Begin to gently insert the catheter into the opening. Guide it upward as if toward the belly button.
Step 7 Once the catheter has been inserted about 2 – 3 inches past the opening, urine will begin to flow.
Step 8 Once the urine flow starts, continue to advance the catheter another 1 inch and hold it in place until the urine flow stops and the bladder is empty.
Step 9 Withdraw the catheter in small steps to make sure the entire bladder empties.
Step 10 Wash the catheter with soap and water. If the catheter is disposable, discard it right away. If it is reusable, rinse the catheter completely and dry the outside. Store the catheter in a clean, dry, secure location.
Change condom and Foley catheters regularly. Condoms are usually changed daily – every other day at the longest. As for a Foley, there is no real guideline for how often it should be changed, but changes are commonly made monthly.
A Suprapubic catheter is typically inserted by a qualified physician or other health-care provider. A trained professional will also change the suprapubic catheter when needed. The individual should discuss when changes should occur with his/her doctor.
KEEPING PERSONAL URINARY CARE SUPPLIES CLEAN
Before you start, you need a:
- cleaning area such as a sink or wash pan
- strong disinfectant solutions such as liquid bleach or Pine Sol
- small funnel or syringe (not required, but it helps to clean inside the bag, connector & tubing, and
- place to hang leg and bed bag for drying.
STEP BY STEP PROCESS FOR CLEANING URINARY SUPPLIES
Step 1 Unplug the dirty bag, tubing and connector from the catheter.
Step 2 Attach a clean bag, tubing and connector to the catheter.
Step 3 Completely empty urine out of dirty bag.
Step 4 Clamp the drainage valve closed.
Step 5 Use a small funnel or syringe to pour a mixture of water and disinfectant solution through the connector and tubing into the bag (1 part disinfectant to 8 to 10 parts water – less water makes for a stronger disinfectant, but too strong a solution can damage your skin on contact).
Step 6 Shake bag gently so solution cleans all parts of the inside of bag.
Step 7 Open drainage clamp to empty solution from bag.
Step 8 Wash off outside of bag with fresh solution.
Step 9 Repeat steps 4-8 using water without solution.
Step 10 Hang bag up to dry.
Clean your urine drainage bag each day, and check your tubing and connectors every 2 to 3 days for sediment buildup. If you see mineral build up after cleaning, soak the tubing and connector in bacteria-killing solution for 6-8 hours. If this does not remove the buildup, replace the tubing or connector.
Keeping skin clean is another important element for maintaining an individual with SCI’s health. First, always wash hands before and after any bladder management method. To care for the indwelling catheter (Foley or Suprapubic), cleanse the urethral area (where the catheter exits the body) and the catheter itself with soap and water every day. After removing a condom, wash the entire genital area with soap and water before putting on a new condom. Finally, change clothes and wash well immediately after any urine leakage or bowel movements.
Getting a yearly medical check-up should be a part any individual’s long-term care plan. The check-up should include a urologic exam to see that the individual’s urinary system is healthy. This usually includes a renal scan or ultrasound to determine whether or not the kidneys are working properly. The exam may also include an X-ray of the abdomen (KUB). This check-up helps the doctor ensure that the individual’s urinary system is acting appropriately and identify other potential problems as early as possible.
POTENTIAL URINARY COMPLICATIONS
Most complications can be avoided with proper urinary system care. However, individuals with SCI are likely to develop a urinary tract infection (UTI) even with the best bladder care. Not only are individuals with SCI at high risk for UTI, but complications due to UTI are also the #1 medical concern and more likely to affect their overall health and health care costs.
Bacteria are tiny, microscopic single-celled life forms that group together and form colonies. Different bacteria can live in various systems of the body. Those bacteria living in the urinary system can quickly multiply and lead to infection or disease.
Individuals with SCI should watch for early signs of an infection such as sediment (gritty particles) or mucus in the urine; cloudy urine; bad smelling urine (foul odor); and blood in the urine (pink or red urine). Attempt to avoid the onset of an infection by drinking more water; avoiding beverages with sugar, caffeine and alcohol; and emptying the bladder more often.
Antibiotics are used if an individual suffers an infection. Antibiotics are prescribed by a doctor and essentially kill the “bad” bacteria causing the infection. Always follow the doctor’s advice on treatment of UTIs. On the other hand, many doctors do not know that individuals with SCI have special considerations when it comes to the use of antibiotics for UTIs. In order to properly treat an individual with an SCI for urinary complications the treating doctor needs to have experience and familiarity treating those with SCIs. The doctor should know that most (80%) individuals with SCI have bacteria in the urinary system at any given time. The presence of bacteria is common because bacteria from the skin and urethra are easily brought into the bladder with ICP, Foley, and Suprapubic methods of bladder management.
Also, many individuals with SCI are not able to completely empty their bladder, leaving some bacteria in the urine remaining in the bladder. Whereas bacteria identified in a urine culture is commonly cause for treatment by doctors, you do not necessarily need treatment for an infection. Antibiotics are only recommended for treatment of UTIs if you actually develop one or more symptoms of infection that include: fever; chills; nausea; headache; change in muscle spasms; and autonomic dysreflexia (AD). Depending on your level of injury, you may also feel burning while urinating or discomfort in the lower pelvic area, abdomen, or lower back.
When you show symptoms of illness, it is highly recommended that you get immediate advice on treatment from your doctors. Your doctor should also get a urine sample prior to prescribing a treatment. These two actions are recommended so that your doctor can first rule out any other health problems. Second, your doctor can prescribe the most effective antibiotic to treat your specific infection (bacteria type). Finally, antibiotics should be taken exactly as prescribed and for a sufficient duration to fully kill the bacteria.
Use of antibiotics as a preventative measure for UTIs is not recommended unless there is an overriding medical need to prevent an infection. Although there are some circumstances such as pregnancy, when prevention of infection is needed to avoid unwanted medical complications, antibiotic resistance is a major concern for individuals with SCI. Each time you take an antibiotic, the bacteria have the opportunity to change in some way that reduces or eliminates the effectiveness of that antibiotic to kill the bacteria in the future. So it becomes harder and harder to get an effective antibiotic when you actually get sick from a bacterial infection. Whereas bacteria found in the urinary system can cause illness, there are also “good” bacteria found in your digestive system. These bacteria are actually beneficial for maintaining the natural balance of organisms (microflora) in the intestines. Maintaining this proper bacterial balance can help individuals with SCI in their bowel management.
Anytime antibiotics are taken, these medications kill both the good and bad bacteria. Therefore, probiotics are sometimes recommended by doctors during and/or after a course of antibiotics to replenish and restore the numbers of beneficial bacteria lost to antibiotic use. Probiotics are dietary supplements containing potentially beneficial bacteria or yeast. The most common sources for probiotics are yogurt, but other dairy products such as cheese, milk, sour cream and kefir are also probiotics. Although it is likely that a UTI is present when symptoms of illness have been observed, it is possible that the individual may have another health problem. Therefore, it is highly recommended that individuals who show signs of UTI call their doctor immediately for advice on treatment if you develop any symptoms. It is recommended that you provide your doctor with a urine. These two actions are recommended so that the doctor can rule out any other health problems and prescribe the most effective antibiotic to treat the individual’s specific infection (bacteria type).
If an individual becomes ill with two or more UTIs per year, it can be an early sign of other problems with the urinary system. A complete urologic examination may be necessary to find out if a more serious problem is present. Individuals may want to consult with a urologist, a doctor specializing in the treatment of the urinary system.
Remember, any doctor who treats an individual with SCI should be familiar with the medical issues of individuals with SCI. Kidney (Renal) failure was once the leading cause of death for individuals with SCI. Today, improved methods of bladder management have resulted in fewer and less severe complications with the kidneys. A more common cause of death related to the urinary tract is now sepsis (a blood stream infection resulting from a symptomatic infection in the urinary tract). Kidney and bladder stones can form in the urinary system. Such stones usually hinder the kidney/bladder functions and can cause infection. Most individuals with lower levels of injury will notice pain associated with a stone. Those with higher levels are not likely to feel the pain. Blood in the urine is also a common sign that a stone has developed. If an individual experiences reoccurring or prolonged symptoms of AD that seem to be without cause, it may also be a sign of a kidney stone.
Urine leakage or incontinence is a problem for some individuals. Treatment can include both drugs and surgery. Medications are often used to control bladder spasms and tighten the sphincter muscles. Several surgical options are available for treating urine leakage. A new urinary reservoir (“pouch”) is made from bowel tissue. The ureters are implanted into the new bladder “pouch.” The urine is drained with a catheter through an opening (stoma) in either the navel or stomach wall. Another surgical method is bladder augmentation cystoplasty. Here the bladder is enlarged using bowel tissue. Since surgery involves both the urinary and gastrointestinal systems, recovery time is longer.
Bladder cancer is another concern for some individuals with spinal cord injury. Research in aging with SCI shows a small increase in the risk of bladder cancer among individuals with SCI who have been using indwelling catheters for a long period of time. Smoking further increases this risk. If you have used an indwelling catheter for at least 10 years, it is strongly recommended that you have regular cystoscopic evaluations. Treating other problems of the urinary system is important. Many times these problems do not have any symptoms. This means they can go undetected until the problem becomes serious. The annual physical exam and laboratory studies are the best ways to find problems early and treat them before they become serious.
The keys to a healthy urinary system are taking all the proper steps to prevent complications and identifying any complications as early as possible for treatment. This includes learning proper bladder management techniques as well as proper bladder care. Learning these skills will allow an individual to improve the chances for lasting long-term health.
BOWEL MANAGEMENT
 THE DIGESTIVE SYSTEM
THE DIGESTIVE SYSTEM
The digestive system has both upper and lower digestive tracts. The upper digestive tract breaks down the food that you eat into the nutrients that fuel your body. The digestion of waste begins in the lower tract small intestine and large intestine. In a wave-like action called peristalsis, the waste is moved through the large intestine where water is removed, resulting in the left-over stool. A bowel movement (BM) is normally initiated when enough stool collects in the rectum. The urge to empty the bowels intensifies as the rectum fills with stool. When going to the bathroom, the brain then signals the release of the anal sphincter muscle, and muscle action pushes the stool out through the anus. The frequency between each BM normally differs greatly among people. Some people will normally have 1 to 3 movements per day. Normal frequency for some people can be as few as 3 times a week. Normal consistency of the stool can also vary. Although a normal BM should be easy to pass, some people may have harder or softer stools than others.
FOLLOWING SPINAL CORD INJURY
Following spinal cord injury (SCI), messages from the body are not able to reach the brain like before the injury. This usually means a loss of sensation that the bowels are full and the “urge” to empty the bowels is no longer there, and loss of voluntary sphincter muscle control. When normal bowel function is lost due to an injury to the nervous system (spinal nerves), bowel function is commonly referred to as a neurogenic bowel.
In general, two types of neurogenic bowel can occur after SCI. The type depends on the level of injury. A reflex bowel is common with injuries above T-12 (Upper Motor Neuron injuries). With a reflex bowel, the anal sphincter remains closed. However, a reflex BM can still occur at any time and without warning when the stool fills the rectum. With injuries below T-12 (Lower Motor Neuron injuries), there is usually a loss of reflex response, or flaccid bowel. Although there is reduced peristalsis and a loss of anal sphincter tightness with a flaccid bowel, the bowel does not usually empty itself. However, the loose sphincter means mucus and fluid can seep around stool and leak out the anus.
BOWEL PROGRAMS
Stool absolutely must be removed regardless of the level of injury, and thus a bowel program based on the individual’s bowel type will be necessary.
A REFLEX BOWEL PROGRAM may be done daily, every other day, or even as few as 3 times a week. There are 8 general steps in a reflex bowel program:
Step 1 Wash hands thoroughly.
Step 2 Prepare your supplies. You will need:
- gloves (powder and latex free are preferable)
- lubricant (water-based or anesthetic only)
- toilet paper and/or blue under pads (Chux)
- stimulant (Enemeez® mini-enemas or Magic Bullet Suppositories® are generally accepted for regular use by individuals with SCI)
- assistive devices (a suppository inserter, finger extension, and digital stimulator)
Step 3 Get into a comfortable position. When possible, it is best if you sit on a toilet or commode chair so that gravity can help move the stool down and out. If you cannot sit, lay on your bed with your body turned on the left side. Use under pads (Chux). Do not use a bed pan because it may damage your skin.
Step 4 Manual stool removal. The lining of the rectum is delicate. Insert a gloved, lubricated finger into the rectum and gently hook your finger around any reachable stool and remove it from the rectum.
Step 5 Insert a rectal stimulant. Methods for insertion include using a gloved hand to squirt the lubricated mini-enema as high as you can into the rectum. Likewise, place the lubricated suppository high into the rectum, leaving the suppository touching the wall of the rectum.
Step 6 Digital rectal stimulation. Sometimes referred to as “Digi-stim,” this process promotes peristalsis and the relaxation of the sphincter muscle. A good time to begin digital rectal stimulation is once the stimulant starts to act. Mini-enemas will probably start to act within 15 to 20 minutes after the insertion. The suppository will probably start to act within 20 to 30 minutes after insertion. Passing of gas or stool may also indicate a readiness for digital stimulation. Insert a gloved, lubricated finger into the rectum and gently start moving your finger in a circular pattern for 20 to 30 seconds, keeping the finger in contact with the rectal wall. Repeat the process every 5 to10 minutes until the BM is complete.
Step 7 The individual must be able to recognize when the BM is over. Indications that the BM has been completed include determining that there is no more stool after 2 consecutive digital stimulations; mucus coming out without any stool; or if the rectum is closed tightly around the finger.
Step 8 Clean up. Wash and dry the anal area.
A FLACCID BOWEL PROGRAM is usually done one or more times daily. There are 6 general steps in a reflex bowel program:
Step 1 Wash hands thoroughly.
Step 2 Prepare your supplies. You will need:
- Gloves (powder and latex free are preferable)
- Lubricant water-based only)
- Toilet paper
Step 3 Get into position. Most individuals with a flaccid bowel are able to sit on a toilet or commode chair.
Step 4 Manual stool removal. Stimulants are not usually effective for a flaccid bowel, so manual removal of stool is done (as with reflex bowel) about every 5 minutes until the BM is over. Between each 5 minute removal time, you can promote stool movement by utilizing digital rectal stimulation (as with reflex bowel); firmly rubbing your abdomen in a clockwise direction with your hand; and movement of the body. The most commonly utilized body actions are leaning forward and side-to-side; body push-ups to reposition and vary pressure areas; tightening and releasing of abdominal muscles; “bearing down” to force stool out (known as a valsalva maneuver and should be avoided if you have a heart condition); and inhaling air deeply followed by forcing air out by increasing abdominal pressure.
Step 5 Know when the BM is over. The BM is probably over when you have no stool results after 2 manual removals, which is about 10 minutes without results.
Step 6 Clean up. Wash and dry the anal area.
BOWEL MANAGEMENT
Bowel management is essentially the ability to maintain control over bowel movements. Bowel control includes the ability to retrain the bowel to empty at a planned, regularly scheduled time; avoid accidental, unplanned BMs; avoid leakage between each bowel program; maximize stool removal during each bowel program; maintain normal stool consistency; finish each bowel program within a reasonable time (within 60 minutes); feel secure to fully participate in all desired activities of daily living; and keep your body’s digestive system healthy. A properly designed bowel program is only 1 element of bowel management. Other essential elements to a successful bowel management program include:
- Schedule: Before the SCI, an individual’s body was probably trained to have bowel movements that were fairly predictable. For example, you may have had a BM each morning at roughly the same time of day or every other day. Following injury, the individual must essentially retrain the body to respond with a BM only when stimulated during your bowel program. Individuals will need to select a time of day when having a BM best fits your lifestyle. If it is at all possible, individuals should maintain the same schedule that was implemented at the beginning of rehabilitation. Individuals should attempt to follow this schedule until they are accident free between multiple bowel programs. Once your body has adjusted and is well trained to respond with a BM only when stimulated, you may then adjust your bowel program schedule if needed. For example, you may prefer to change your bowel program from morning to night or choose to perform a bowel program every other day instead of every day. Whether you change your schedule or not, you should be able to eventually feel fairly secure in maintaining a regular, predictable bowel program.
- Nutrition: When and what you eat greatly influences your bowel program. For example, eating a meal, high fiber snack, or drinking a warm liquid (such as hot tea, hot apple cider, etc.) initiates peristalsis in a reflex bowel. If you eat or drink something warm about 30 minutes prior to starting your bowel program, you will likely have more effective results. Your fiber intake helps maintain the health of your entire digestive system. Although some individuals take a fiber supplement, vegetables, fruits and whole grain foods are the recommended sources for getting your daily fiber intake. You need about 25 to 35 grams(g) of fiber each day. However, you need to gradually make changes to your fiber intake because sudden increases in fiber intake can cause diarrhea and decreases in fiber intake can cause constipation. Some foods, especially eaten in excess, are more likely than others to cause common bowel problems. For example, dairy products, white potatoes, white bread and bananas can contribute to constipation. Fruits, caffeine and spicy foods can cause diarrhea. Beans, corn, onions, peppers, radishes, cauliflower, sauerkraut, turnips, cucumbers, and apples can cause excessive gas buildup.
- Water: Water should be your beverage of choice for many reasons. A big reason is that water helps regulate your body’s digestive system, keeps your stool from getting too hard, and prevents constipation and impaction. Although fresh vegetables and fruits are good sources for water as well as fiber, you still need to drink the proper amount of water. Generally, your bladder management method will determine how much water you typically need daily.
- Physical Activity: Engaging in physical activity promotes easier passage of food through the digestive system.
- Medications: Many over-the-counter and prescription medications can impact your bowel program. These include bowel-related medications that you take by mouth (orally) or by suppository, and some medications that you take for other reasons can influence your bowel function. Therefore, you should always talk with your health care provider before taking any medication. Constipation and diarrhea are common side-effects of medications. For example, codeine, ditropan, probanthine, and aluminum-based antacids can cause constipation. Magnesium-based antacids can cause diarrhea. Stool softener and laxative use are common among individuals with SCI. Although Colace® (stool softener) and Peri-Colace® (stool softener with added laxative) are mild and may be well tolerated by most people, too much or too little dosage may result in diarrhea or constipation.
- Regularity: Every individual with SCI is unique, but you will likely agree that an unplanned BM is one of the most embarrassing things that can happen. Your best chance to avoid accidents is with consistent bowel management and established bowel program. For example, you should maintain your routine even if your normal routines get interrupted by travel, sickness or the like. If you have an unplanned BM, you still need to continue your bowel program when it is scheduled. Individuals should consult with their doctor when adjustments to the bowel program are necessary.
COLOSTOMY
A colostomy is a surgically-created hole leading from the large intestine to the outside of the abdomen. Typically, a bag is placed over the abdomen hole to collect the stool before it gets to the rectum. Do not necessarily rule out a colostomy on first thought. This procedure is becoming more popular among individuals with SCI, especially people with constant bowel problems. In such cases, a colostomy can greatly improve quality of life. To determine whether a colostomy is a helpful treatment option for a given individual, begin by researching colostomy use and how it works as a bowel program option. If it is an option of interest, attempt to speak with someone with SCI who has one. Then, talk to a physiatrist (doctor in rehabilitation medicine) to discuss whether a colostomy is a good option for the particular individual.
RESPIRATORY MUSCLES
The respiratory system, also known as the pulmonary system, is used for breathing. The windpipe and lungs are the two main parts of the respiratory system. When you inhale, or breathe air in through your mouth or nose, oxygen travels down your windpipe and into your lungs. Your lungs then filter the oxygen and send it through your blood stream to all of your body parts. When you breathe out, or exhale, you send the left over carbon dioxide out of your body, through your windpipe and out of your mouth or nose.
When you exhale, it does not require any effort from the body’s muscles. However, you normally use a combination of four respiratory muscle groups to breathe air into your body. The diaphragm, a strong, dome-shaped muscle that separates the abdominal and chest cavities, is normally the main muscle that you use when you inhale. The intercostal muscles are located between the ribs. These muscles help to expand your ribs as you inhale. The neck muscles normally work to expand your upper chest when inhaling. The abdominal muscles work with these other muscle groups to help you breathe deeply and cough.
The brain normally sends signals through nerves in the spinal cord to control the four respiratory muscle groups. When everything is working properly, the pulmonary system and respiratory muscles work together allowing you to breathe in and out without much effort. In fact, most people breathe without ever thinking about it.
AFTER SCI
The windpipe and lungs are not typically affected by a spinal cord injury. However, respiratory problems may occur when the signals sent from the brain can no longer flow through the spinal cord to control the respiratory muscles. The amount of muscle control that is lost after a spinal cord injury depends on the level of the injury, along with the completeness of the injury.
Individuals with injuries below the T12 level do not usually lose any control of the four respiratory muscle groups needed for breathing. This means the respiratory system is not usually affected by injuries in the lumbar or sacral regions of the spinal cord. Individuals with complete thoracic or cervical injuries do experience a loss of their respiratory muscle control. The higher the level of injury, the greater the loss of respiratory muscle control.
Complete injuries in the thoracic or cervical regions usually result in the permanent loss of respiratory muscle function below the level of injury. However, if that injury is incomplete, it is impossible to predict whether individuals will regain some or all of their respiratory function below the level of injury. Injuries in the thoracic area (T1-T12) of the spinal cord affect the control of the intercostal and abdominal muscles. A lower level of injury, such as a T10, results in the individual losing a small amount of muscle control. With a higher level of injury, such as a T2, individuals will lose most of their intercostal and abdominal muscle control. Complete injuries in the cervical region usually result in a total loss of intercostal and abdominal muscle control.
Again, the higher the level of injury, the greater the loss of additional muscle controls. For example, a complete injury between levels C3 and C5 loses all control of the diaphragm muscles. With a complete injury at level C3 and higher, the individual loses control of all four muscle groups that are needed for breathing. A ventilator is then needed to assist in breathing. The ventilator does the work of the absent muscles and forces air into the lungs. Many people with a C4 level of injury, and even some people with a C3 level of injury, can eventually breathe without the aid of a ventilator or may only need it for part-time assistance. Those individuals with complete injuries above C3 need a ventilator for full-time assistance.
RESPIRATORY COMPLICATIONS
Individuals with a spinal cord injury are at increased risk for developing respiratory complications. Any loss of respiratory muscle control weakens the pulmonary system, decreases one’s lung capacity, and increases respiratory congestion. It does not matter what the level of injury is or if the injury is complete or incomplete. However, the risk for complications is greater for individuals with a complete injury and for persons with tetraplegia.For persons with high level tetraplegia (C5-C1), ventilatory failure is a common complication after injury. The person typically lacks the ability to breathe without assistance.
Another common problem is atelectasis. This is when the lungs partially collapse because not enough air is getting into them.
Persons with all levels of injury are at risk for pulmonary embolism. Pulmonary embolism is a blockage in the blood vessels of the lungs by a blood clot, and it is the second leading cause of death for persons with SCI within the first year after their injury. In addition, individuals with high tetraplegia (C1-C4) are about 100 times more likely to die from diseases of pulmonary circulation, regardless of time after injury, when compared to the general population. Those individuals with paraplegia (T1-S5) are almost 50 times more likely to die from pulmonary embolism. Ventilatory failure, atelectasis and pulmonary embolism are all very serious, life-threatening respiratory complications.
However, pneumonia is the leading cause of death for all persons with spinal cord injury. This is true regardless of your level of injury or how long you have been injured. Be aware of the symptoms for pneumonia. They include shortness of breath, having pale skin, a fever, along with a feeling of heavy chest, coughing, and an increase in congestion. If you have symptoms of pneumonia, call a doctor immediately for advice on treatment.
PREVENTION OF RESPIRATORY COMPLICATIONS
- Because persons with SCI are more likely to develop respiratory complications within the first year after injury, it is very important to take steps to prevent complications during the acute care and rehabilitation stays.
- Treat all symptoms of respiratory complication aggressively to help prevent further complications from developing.
- Individuals with SCI should receive a yearly vaccination for (pneumococcal) pneumonia and influenza.
- Avoid the buildup of secretion in the lungs. It can be helpful for persons with high level tetraplegia to receive regular treatments with a cough assist machine. Individuals with tracheotomies who are on a ventilator need to have secretions suctioned from their lungs on a regular basis
LONG-TERM CARE
Individuals with SCI should also have an ongoing, life-long plan to help prevent respiratory complications. Maintain proper posture and mobility and sit up in your wheelchair everyday and turn regularly in bed to prevent buildup of congestion. Coughing regularly is a useful technique in avoiding respiratory complications; individuals can use machines to help them cough, have someone perform manual assist coughs, or perform self-assist coughs. Individuals should wear an abdominal binder to help assist the intercostal and abdominal muscles.
Individuals with SCI should attempt to follow a healthy diet and manage their weight. Weight management is important because respiratory problems are more likely to occur if an individual is too underweight or too overweight. Drinking plenty of water is important because doing so helps the body in many ways, and water helps to keep congestion from becoming thick and difficult to cough up.
Do not smoke under any circumstances! Smoking not only causes cancer, but other harmful effects include a decrease of oxygen in the blood, an increase in congestion in the chest and windpipe, a reduction in the ability to clear secretions from your lungs, a destruction of lung tissue, and an increase in the risk for respiratory infections such as pneumonia and bronchitis.
Live sensibly by avoiding close contact with people who may have a cold or flu and avoid areas with dust, smog and other air pollutants. See a doctor at least once per year. The doctor may recommend that the individual receive a chest x-ray or a flu shot.
Exercise is another critical element to avoiding respiratory complications. Every individual with SCI can benefit from some type of exercise. However, it is important to first talk to your doctor to find the right exercise program. Participation in athletics and other cardiovascular activities can improve strength and endurance while helping to keep the pulmonary system strong. If an individual suffers from a high level of injury or does not like strenuous exercise, it may be helpful to do breathing exercises.
Here are five breathing exercises that you can do at least two times a day to help your pulmonary system.
- Take a deep breath and hold it for a few seconds before slowly breathing out.
- Take a deep breath bringing in as much air as you can and as fast as you can before pushing the air out as fast as you can.
- Take a deep breath and hold it, take another breath and hold it, and take one more before slowly breathing out.
- Take a deep breath in then breathe out counting as long and as fast as you can.
- If you have a spirometer, use it to both exercise and keep a measurement of your progress.
BLOOD CLOTS AND CIRCULATION
With a spinal cord injury, being immobile for long periods of time slows blood circulation and can cause clots to form. Blood-thinning medications, leg pumps, and special stockings, can help improve circulation and prevent fluid build up.
An individual living with a spinal-cord injury may experience muscles spasms which cause their limbs to twitch or “jump”; this is relatively rare and unfortunately it is not an indication that the person is regaining sensation or movement in those areas. These involuntary movements occur because some nerves have become more sensitive, yet the damaged spinal cord will not allow the brain to interpret and regulate these nerves’ signals.
PERSONAL CARE ATTENDANT
Between 40 and 45 percent of individuals with spinal cord injuries (SCI) need personal assistance with some daily activities. It is understandable that the majority of persons needing assistance have higher levels of injury. They may need personal care assistance with getting in or out of bed, managing bowel and bladder issues, bathing and dressing. Some individuals may need someone to drive, shop and clean for them too. However, there is also a growing percentage of persons with lower levels of injury needing assistance as they get older. They may need assistance with household activities as they grow older and experience increased pain or fatigue.
Most Personal Care Attendants (PCAs) need education and training on general issues associated with SCI. Even if you find a PCA with a lot of experience, you yourself have unique needs. Although all issues are important, your bowel, bladder, skin, and respiratory care must be understood by your PCA. Communicate your bowel and bladder needs clearly. Make sure you stress the importance of daily skin care, and your PCA should know how to conduct daily skin checks and spot problems.
PCAs need to know about respiratory sickness too. Flu and pneumonia can be life-threatening for most people with SCI. This fact makes it important to have PCAs understand these dangers and work to prevent spreading these conditions. Washing hands should always be done often to help prevent the spread of germs. PCAs who are sick with a cold or flu should avoid contact when possible. If contact is unavoidable, PCAs should wear a mask and wash hands more often. For individuals on a ventilator, PCA training on all the mechanical works of a ventilator can mean life or death. There should also be an emergency plan for ventilator problems and failures.
AFTER A SPINAL CORD INJURY
A spinal cord injury (SCI) is one of the most devastating of all traumatic events. It results in a loss of some or all of an individual’s sensation and movement. It is common for individuals who are newly injured to have health problems. Plus, it takes time to build enough strength to be able to fully participate in daily activities. Individuals who are newly injured will likely experience grief. This is a period of mourning that is similar to that following the death of a loved one. The difference is that you are grieving the loss of your sense of touch along with your ability to walk or use your hands. You will likely experience many different thoughts and feelings after injury. Some may seem extreme and others mild. There is no step-by-step grieving process, but some thoughts and feelings are common after injury.
- Denial/Disbelief: Individuals may first react to your injury as if nothing happened. Individuals may refuse to accept that the loss of feeling and movement is permanent. Instead, individuals may view the injury as an illness similar to a cold or flu that will soon pass with time.
- Sadness: Obviously, no one is happy to be injured, no matter what your level of injury. Extreme sadness is common after injury because you have experienced a great personal loss. Sadness is that down, or blue feeling that you have when something bad happens. However, do not confuse sadness with depression. Depression is a medical condition that requires professional treatment. Individuals may be depressed if experiencing symptoms such as extreme sadness, inactivity, difficulty in thinking and concentrating, a significant increase or decrease in your appetite and/or time spent sleeping, and feelings of dejection, hopelessness or worthlessness. Depression may even involve thoughts about suicide.
- Anger: Some people react to their injury with strong feelings of displeasure. Individuals might lash out verbally or want to become physically violent towards others. Individuals may feel angry toward themselves especially if their actions resulted in the injury.
- Bargaining: At some time following the injury, individuals may begin to admit that their injury is a serious condition. However, individuals may still want to hold onto the belief that the injury is not permanent. While individuals may act as though they accept the injury as “the way things are,” acceptance may come with the belief that they will be rewarded for prayers and hard work in therapy and eventually recover from the injury at some point in the foreseeable future.
- Acceptance: Grieving usually ends as the individual comes to accept a realistic view of their current condition and once again find meaning in life. A sign of acceptance is when individuals begin to think about their future as an individual with SCI and set goals to pursue in life.
ADJUSTMENT TO SPINAL CORD INJURY
Adjustment is defined as adapting to a new condition. Everyone makes adjustments during their lifetime. Some of the conditions that individuals are forced to adjust to may be planned and individuals typically have time to think about how they will react to the situation. For example, individuals may have to make adjustments in work hours when starting a new job. Other events may be a surprise in which individuals are forced to adjust to an unplanned event.
Individuals who adjust well to unexpected events generally lead healthy, active, and happy lives after their trauma. Individuals who do not adapt well to unexpected events tend to be less healthy, less active, and unhappier after their injury. Most individuals experience two primary issues of adjustment to spinal cord injury. Immediately after being injured, it takes time to get use to life after injury. Some people grieve longer than others, so the adjustment period is different for everyone. It may take as much as a year for individuals to accept the realities of the injury. Individuals will also experience a continued process of adjusting to the unique issues that occur in their everyday life as a person with SCI.
PROBLEMS ADJUSTING TO SCI
If an individual has been injured for a year or more and has not come to accept the injury and its consequences, it is a good idea to look into other areas to find out whether or not the problems adjusting to SCI can be addressed. You may find it hard to believe upon first thought, but what happens to you is not as important as what you are thinking when something happens to you. Your thinking directly influences how you feel and react to events that occur in your life. This concept is the basis for Rational Emotive Behavior Therapy (REBT). Many counselors and psychologists teach REBT as a way to help people with and without SCI gain a healthy view of their lives.
HEALTHY ADJUSTMENT TO SCI
No matter what the event, you know that it triggers self-talk. These ideas, thoughts, and/or beliefs lead to your feelings. Your behavior and the results of your behavior are guided by your feelings. One of the biggest keys to adjusting to spinal cord injury is personal motivation. Individuals who are newly injured are often motivated to attend therapy sessions out of a desire to gain strength and function. You probably have a strong belief that your paralysis is only temporary, and you will soon return to your old, “normal” self. This hope is a common reaction after an injury. Unfortunately, it is far more likely for individuals to recover function based on their level and completeness of injury. In fact, only a few people actually fully recover from their injury. This does not mean that all hope is lost for a full or partial recovery. Almost all individuals with SCI continue to hope that they will walk again one day. However, a cure for paralysis may or may not come in your lifetime. A healthy approach to this reality is to move forward with your life after injury with the continued hope that advances in medicine will one day lead to a cure. In other words, do not wait on a cure to proceed with your life!
People who adjust well to life after injury are usually motivated to meet personal goals. These goals are different for everyone and often change throughout life. For example, your goal today may be to get a job, and you may want to have children in the future. Research from the University of Alabama at Birmingham (UAB) shows that people with SCI who are goal-oriented are less likely to be depressed and more likely to obtain some acceptance of their disability than persons who are not goal-oriented. However, it is up to you to find purpose in your life and the motivation to achieve your goals. It may help to think about what you wanted out of your life before you were injured. For example, you may have once strived for good health, an enjoyable job, and a loving family. There is no reason that you cannot continue to strive for the same things now that you have a spinal cord injury.
FAMILY ADJUSTMENT
It is important for individuals with SCI to recognize that the injury also has a tremendous impact on the family. Although they may not have to adjust to losing the use of their hands or ability to walk, family may experience a loss of the way their life was before your injury. For example, they may have to adjust to the role of caregiver. They may need to work to help with family finances. All of the changes that they face can lead to added stress and anxiety.
Family members also grieve. They may ask questions to try and understand the full impact of the injury and to help ease their feelings of sadness and fear. As your family comes to accept the injury, they face issues of adjustment similar to those you may experience. Children are naturally curious and adjust to events by asking questions. They ask questions because they make few assumptions about how the injury impacts their life. Therefore, children adjust rather quickly to an injury if their questions are answered in a clear, honest manner.
PROBLEMS IN FAMILY ADJUSTMENT TO SCI
As an adult family member, you may have difficulty with adjustment if you have your own irrational beliefs about life after injury. For example, you may hold the false assumption that individuals with SCI cannot work. You may hold the unrealistic idea that “no one” with SCI can or “should” have children. You may hold the irrational belief that you “must” do everything for your loved one who is injured.
Your actions as a family member are reflected in what you say and do around your loved one. If your actions are based on irrational beliefs, you may be unknowingly acting with less than supportive behavior. For example, if you continue to do things for your loved one that he/ she can do, your actions may be encouraging your loved one to be overly dependent on others.You may also be reinforcing your loved one’s false assumptions that individuals with SCI should be pitied or felt sorry for because life has treated them unfairly.
You may be enabling your loved one to engage in self-destructive behavior if you ignore or deny the possibility of a problem with substance abuse. Plus, it is also likely that your irrational beliefs will influence your own feelings, which may then lead to unhealthy behavior and unhealthy results. If you experience prolonged feelings of stress and anxiety, you may be putting yourself at risk for serious health problems such as disease or stroke if you do not adjust your views of life after injury
HEALTHY FAMILY ADJUSTMENT TO SCI
If you are a family member, healthy family adjustment is, essentially, taking care of you. For example, you can take time away from your loved one to do those things that you enjoy. You can help minimize your stress and anxiety by working to replace your own false assumptions, unrealistic ideas, and irrational beliefs. You can start by learning the facts about SCI. Then, challenge your irrational beliefs with evidence to dispute your beliefs. Finally, replace your false information with facts. Hopefully, you will soon discover that you too are living a healthier, happier, and more satisfying life.
No matter if you have a spinal cord injury or not, you have control over what you feel by choosing how you want to think about your situation. You can be happy and more hopeful about your life, but it will only happen when you work to make it happen. Your thoughts, feelings, and behavior do not change overnight. It takes time to grieve your loss and come to accept the realities of the injury. Then, you face a continued process of adjusting to everyday issues of living with SCI. If you avoid false assumptions, unrealistic ideas, and irrational beliefs, you will give yourself more opportunities to reach your goals and have the life that you desire.
THE PROBLEM OF PAIN AFTER SCI
Pain is a serious problem for many individuals with spinal cord injuries (SCI). Pain after SCI can occur in parts of the body where there is normal sensation (feeling) as well as areas that have little or no feeling. The pain is very real and can have a negative impact on quality of life. An individual in severe pain may have difficulty carrying out daily activities or participating in enjoyable pastimes.
The majority of individuals with SCI report that they have chronic pain. Chronic pain is pain that does not go away and instead lasts months to years. The cause of the pain may be unknown but is most often related to nerve damage from the SCI or musculoskeletal problems that arise in dealing with an SCI. The pain can come and go. Chronic pain is difficult to completely eliminate but often can be managed or reduced enough so that it doesn’t control the individual’s life.
Chronic pain can cause or worsen psychological problems such as depression, anxiety and stress. This does not mean the pain is “all in your head,” but rather that pain and distress can make each other worse.
Even though pain after SCI can be complicated and difficult to treat, there are many treatments available that can help. Understanding the pain, working with the doctor and being open to a variety of treatments will help to manage the pain and improve quality of life. Many people with difficult chronic pain problems after SCI have found relief using techniques described here.
TYPES OF PAIN
A person with SCI can have many different types of pain in different locations, including areas where there is not usually any feeling. Understanding what type of pain you have is key to choosing and implementing the right treatment. Therefore, your doctor will ask you to describe your pain in a variety of ways, including its locations, severity, how long you have had it, what makes it worse or better and so on. The doctor also may request that the individual undergo tests such as an x-ray or MRI (magnetic resonance imaging).
NEUROPATHIC PAIN
Neuropathic pain (“neurogenic pain”) is caused by abnormal communication between the nerves that were damaged by your spinal cord injury and the brain, where nerve signals that inform your brain how your body feels are interpreted. In neuropathic pain, it is thought that the brain “misunderstands” the signals it is getting from around the area of your injury and causes you to experience pain coming from below where you have little or no feeling. This is why a person can feel neuropathic pain in an area that otherwise has no feeling.
People often use words such as burning, stabbing or tingling to describe neuropathic pain, but neuropathic pain varies a great deal from person to person. It is often very difficult to treat, and frequently a combination of treatments must be used.
- Note: If pain starts years after injury, it may be due to a new medical problem, such as a syrinx, a fluid-filled cavity that forms in the spinal cord. It is rare but may require surgery. Therefore, it is very important to contact a doctor if you notice any new loss of sensation, especially in areas around the level of your injury, and any muscle weakness that doesn’t improve with rest.
MUSCULOSKELETAL PAIN
Musculoskeletal pain is caused by problems in the muscles, joints or bones. It is a common problem for all people as they get older, including those with SCI. Musculoskeletal pain can be caused by injury, overuse or strain, arthritic changes, or wear and tear of the joints, often from wheelchair use (including inadequate support for sitting) and/or transfers. This type of pain typically worsens with movement and improves with rest.
UPPER LIMB PAIN
Upper limb (shoulder, elbow and hand) pain is often caused by overuse of the muscles from doing transfers and pressure relief maneuvers and from pushing a wheelchair. It can occur months or many years after injury. Individuals with higher level injuries who use computers or joysticks for many activities (reading, communicating, environmental controls) may develop pain in the hand, arm or shoulder from overuse. Upper limb pain can make it difficult to transfer safely and perform other activities of daily living.
BACK AND NECK PAIN
Back and neck pain are common problems. In people with paraplegia who have had surgery to fuse their spine, increased motion that occurs just above and just below the fusion can lead to back pain. People with tetraplegia (quadriplegia) may also have back pain, especially if they are able to walk but still have weakness. People who use chin- or mouth-operated joysticks may sometimes develop neck pain.
MUSCLE SPASM PAIN
Muscle spasm pain happens when muscles and joints are strained from spasticity.
VISCERAL PAIN
Visceral pain is located in the abdomen (stomach and digestive area) and is often described as cramping and/or dull and aching. This type of pain can be caused by a medical problem such as constipation, a kidney stone, ulcer, gall stone or appendicitis. Since an individual with SCI may not have the usual symptoms associated with these medical conditions, it is important to consult with a doctor who has had experience caring for SCI patients in order to get a correct diagnosis and treatment.
Pain that comes from a visceral problem is sometimes felt in an area away from the source of the problem. This is called referred pain. One common example is shoulder pain that results from gallbladder disease.
Since pain can have so many different causes there is no single way to treat it. A trial of a combination of drugs, therapy and other treatments, including psychological treatments may be necessary.
PHYSICAL TREATMENTS AND INTERVENTIONS INCLUDING ACTIVITY MODIFICATION
Changes in mobility equipment (wheelchair, sliding board), wheelchair pushing and transfer techniques, and in the way the individual performs pressure reliefs can significantly decrease pain in the muscles and joints. Exercises that strengthen and balance joints can also help reduce musculoskeletal pain.
Physical therapy is used to treat musculoskeletal pain. Stretching and range of motion exercises may help relieve pain associated with muscle tension. Exercises that strengthen weak muscles can restore balance in painful joints and reduce pain.
Therapeutic massage may help relieve musculoskeletal pain due to muscle tightness and muscle imbalance.
Acupuncture is used to treat musculoskeletal pain. Tiny needles are inserted into the skin at specific points on the body. This method is thought to work by stimulating the body’s pain control system or by blocking the flow of pain.
Transcutaneous electrical nerve stimulation (TENS) is sometimes used to treat musculoskeletal pain. Electrodes are placed on the surface of your skin and send low levels of electrical current into your body. The current blocks signals from the areas of nerve damage that are triggering a pain response.
PSYCHOLOGICAL TREATMENTS FOR MANAGING PAIN AFTER SCI
Individuals can learn to use psychological techniques to help them manage their pain better to ensure that the pain doesn’t take over their lives. Psychologists trained in pain management can help with a variety of techniques proven to be effective in reducing the intensity and impact of pain.
- Relaxation techniques and/or biofeedback designed to teach you how to reduce muscle pain tension and “mental tension” associated with pain can be helpful in self-management.
- Self-hypnosis training has proven helpful for reducing chronic pain in some individuals.
- Cognitive restructuring. Learning how to think differently about your pain and its effects can actually lead to changes in brain activity and, in turn, the experience of pain.
- Individual psychotherapy designed to help identify desired goals and increase pleasure and meaning in daily life can help reduce pain. Therapy can also help if there is a significant amount of anxiety associated with pain.
MEDICATIONS
There are many different medications to treat pain. All of the medications listed below have shown some success in reducing pain, but none do so completely in every instance. All have possible side effects, some of which can be serious. Discuss all side effects with your doctor. Sometimes combinations of drugs work better than a single drug.
- Non-steroidal anti-inflammatory drugs (also known as NSAIDS) such as aspirin, ibuprofen (Motrin, Advil) and naproxen (Aleve) are most commonly used to treat musculoskeletal pain. Side effects may include stomach upset or bleeding problems.
- Anti-seizure medications such as gabapentin (Neurontin) and Pregabalin (Lyrica) are used to treat neuropathic pain. Side effects include dizziness, sleepiness and swelling.
- Antidepressants are used to treat neuropathic pain and depression. These medications include selective serotonin norepinephrine reuptake inhibitors (SSNRIs), such as venlafaxine (Effexor), and tricyclics, such as amitripltyline (Elavil). Side effects include dry mouth, sleepiness, dizziness and (with SSNRIs) nausea.
- Narcotics (opiates) such as morphine, codeine, hydrocodone and oxycodone are used to treat neuropathic and musculoskeletal pain. These drugs have many side effects, including constipation and sleepiness, and can be habit forming. It is possible to develop dependency on these drugs and some individuals may have withdrawal symptoms after suddenly stopping their dosage. However, these drugs can be used effectively for many individuals, and while not the first consideration for chronic pain management, should not be dismissed because of fears about dependency or side effects.
- Muscle relaxants and anti-spasticity medications such as diazepam (Valium), baclofen (Lioresal) and tizanidine (Zanaflex) are used to treat spasm-related and musculoskeletal pain. These may be taken by mouth or delivered directly to the spinal cord through an implanted pump (see “Intrathecal pumps” below). These drugs can cause sleepiness, confusion and other side effects.
- Topical local anesthetics such as lidocaine (Lidoderm) are used to treat pain that occurs when skin is lightly touched (called allodynia).
- Dorsal column stimulator is used to treat neuropathic pain due to nerve root damage. A high frequency, low intensity nerve stimulator is surgically placed in the spinal canal next to the spinal cord or nerve roots.
- Intrathecal pumps are used to treat neuropathic pain (using morphine) or muscle spasm-related pain (using baclofen) A pump containing morphine or baclofen is surgically placed under the skin in the abdomen. It delivers the medication directly to the spinal cord and nerve roots.
- For more information on prospective surgical treatments and the advance in technology for surgical procedures designed to treat SCIs click here: http://www.beltlawfirm.com/2013/10/will-technology-enable-timely-spinal-surgery-to-occur-throughout-the-state/
- Get treatment for medical problems. Overall health can have a big impact on pain. Urinary tract infections, bowel problems, skin problems, sleep problems and spasticity can make pain worse or harder to treat. Staying as healthy as possible can help reduce pain.
- Try to get as much exercise as possible. Getting regular physical activity can reduce pain as well as improve mood and overall health. It can also be enjoyable and distract you from pain. Your health provider can help you choose physical activities that are safe and appropriate for you.
- Get treatment for depression. Depression can make pain worse. It is best treated through counseling and medication. Getting treatment for depression can help individuals cope with chronic pain and improve the quality of life.
- Reduce stress. Stress can make pain worse or make the pain harder to cope with. Individuals can learn to effectively manage stress through counseling and learning techniques to help you reduce stress and tension, such as relaxation training, biofeedback and hypnosis. Exercise also helps reduce stress.
- Distract yourself. Distraction is one of the best methods for coping with chronic pain. Participating in enjoyable and meaningful activities can help reduce pain and help individuals feel more in control of their lives, especially when pain is at its worst. When individuals are bored and inactive, they have a tendency to focus more on pain, and this can make the pain feel even more debilitating.
- Keep a record. All individuals’ pain is different. Keep a record of what improves the pain and what makes pain worse. Understanding things that affect the pain will help to find effective ways to reduce your pain.
- Get a wheelchair seating evaluation. Poor posture and improper seating can cause serious pain problems. Individuals with SCI should have their seating evaluated by a physical therapist who specializes in wheelchair seating. If an individual uses a manual wheelchair, try to get a high-strength, fully customizable chair made of the lightest material possible (aluminum or titanium). Learn the proper wheelchair propulsion (pushing) technique from a physical therapist.
- Do not use alcohol to ease pain. Using alcohol as a pain medication can lead to alcohol abuse and other serious problems. Some medications should not be mixed with alcohol. Ask your doctor about drinking alcohol, and always read the labels of your prescriptions.
FINDING HELP
If you have pain, it is important to get treatment for it. The ideal source of help would be a physician and psychologist familiar with SCI and pain management, working together. If you do not have easy access to such experts, the next best alternative is to seek help from a multidisciplinary pain clinic where physicians and psychologists are available. Work closely with a health care provider with whom you are comfortable and who understands your condition. Chronic pain is not hopeless. Try not to become discouraged if one treatment doesn’t work, and be open to trying a variety of different techniques. While complete relief from pain may not be possible, living better despite pain is a realistic goal.
Autonomic Dysreflexia
WHAT IS AUTONOMIC DYSREFLEXIA?
Autonomic dysreflexia (AD), also known as hyperreflexia, is a condition unique to people with spinal cord injury (SCI). The condition occurs because the pathway for nerve signals is damaged following injury. Although persons with T6 levels of injury and above are at the highest risk for AD, it does rarely occur in persons with lower levels of thoracic injuries. AD occurs as a response to some type of irritation below the level of injury. The body tries to send signals to the brain to identify and respond to the irritant, but signals are blocked by the SCI. Without communication between the brain and body, blood vessels begin to narrow and cause a rise in blood pressure. When sensors tell the brain that the blood pressure is getting too high, the brain then tries to lower the blood pressure by sending out three signals to:
- Signal 1 – slow the heart rate (A slow heart beat is called bradycardia.)
- Signal 2 – enlarge blood vessels above the level of injury to hold more blood. This causes the upper body to look flushed or red and blotchy.
- Signal 3 – stop squeezing the blood vessels in the legs and abdomen.
- However, signal 3 is blocked by the SCI, so the blood vessels keep squeezing. The blood pressure stays high. It may even keep rising. When the blood pressure gets too high, it can result in a stroke, seizure or death.
SIGNS AND SYMPTOMS OF AD
An individual may have one or more of the following signs or symptoms when experiencing an episode of autonomic dysreflexia. Symptoms may be very slight or even absent, despite a high or even very high blood pressure. Some of the more common symptoms are:
- Pounding Headache
- Blurred Vision
- Flushed Face
- Nasal Congestion
- Red Blotches on Upper Body
- Nausea
- Cool, Clammy Skin
- Chills Without Fever
- Apprehension or Anxiety
- Sweating Above the Level of Injury
- Goose Bumps Above the Level of Injury
- Slow Pulse
WHAT TRIGGERS AD?
- AD is usually caused by something that might ordinarily be painful, uncomfortable or physically irritating. The irritant can be anywhere below the injury level, but the source of AD is usually in a few common areas.
- Bladder issues are the most common causes of AD. It may be bladder overfilling due to a blockage in the urinary drainage device, inadequate bladder emptying, bladder spasms, or possibly stones in the bladder. A urinary tract infection (UTI) can also cause AD.
- Bowel issues are the second most common cause of AD. It can be an overfull bowel, constipation, or bowel blockage (impaction). Any stimulus to the rectum, such as digital stimulation, can trigger a reaction, leading to AD. Certain abdominal tests, such as a barium enema or sigmoidoscopy, can also cause AD.
- Skin conditions such as irritations, wounds, pressure ulcers, and burns (sunburn) are possible causes. Insect bites and ingrown toenails can be triggers. Other possible causes include hard or sharp items that injure the skin, as well as tight, restrictive or wrinkled clothes. Additional triggers can vary greatly.
- Sexual activity and overstimulation can trigger AD.
- Severe abdominal conditions like gastric ulcers and appendicitis are possible triggers.
- Broken bones or even extreme changes in temperature can trigger AD.
- For women, menstrual cramps, pregnancy, labor, and delivery are potential causes.
AD TREATMENT
If an individual suffers from an episode of AD, find and eliminate the cause. The first and most important step is to get into and stay in a seated position. If lying down is unavoidable, keep the head raised as high as possible. Second, check for causes of the AD, and correct any problem issue. Individuals will notice a rapid drop in blood pressure and relief in signs and symptoms when the cause is corrected. Bladder issues are the most common causes of AD, so check these potential problems first.
- Is your drainage bag full?
- Is there a kink in the tubing?
- Is the drainage bag raised higher than your bladder?
- Is the catheter clogged or plugged?
After correcting any obvious problems, individuals should change their catheter if it is not draining within 2-3 minutes. If self-catheterizing, empty the bladder and check bowel issues next. Perform a digital stimulation and empty the bowel. Stop the procedure if signs or symptoms first appear while doing digital stimulation and resume after the symptoms subside.
Finally, check other areas of concern. Loosen any tight, restrictive clothing as well as any abdominal bands or straps. Check wheelchair, bed and seat cushions for sharp objects that might be pressed into the skin causing an irritation. Be sure to look in pant pockets for keys or other objects that might be pressing on the skin.
There are certain gender specific causes of AD that need to be noted. Men need to see if there is any pressure on the testicles and/or penis, especially during sexual activity. Condom catheters need to be examined to be sure they are not too tight. Women may need to treat cramps due to contractions of the uterus before and during menstruation. Labor and delivery often will trigger AD so it is wise to be prepared in case of an episode.
AD AND MEDICATIONS
Medications are generally used to treat Autonomic Dysreflexia only if the cause cannot be found and removed or when an episode continues even after removal of the suspected cause. The medications used to treat high blood pressure (also known as Hypertension) fall into two categories of Antihypertensives. Immediate medications such as Nitroglycerine Paste and Nifedipine (Procardia) rapidly lower blood pressure by widening the blood vessels to make it easier for blood to flow through them and easier for the heart to pump.
Preventative medications are used in cases of recurring AD. For example, a person who has a kidney stone may continually have high blood pressure until the stone is removed or passed. Other medical procedures or events such as child delivery can cause AD, as noted earlier. In these and other cases, you doctor may use medications to prevent AD from occurring.
Men taking medications for erectile dysfunction (ED) may have side effects (flushing in the face, headaches, nasal congestion and/or changes in vision) that also resemble signs and symptoms of AD. A blood pressure check is the best way to tell if you are having an episode of AD or side effects of the ED medication. Higher than normal blood pressure is an indication that you are experiencing an episode of AD, which is cause for you to immediately stop all sexual activity.
PREVENTION
As with most secondary conditions in SCI, prevention is the key. Since we know what some of the triggers are for Autonomic Dysreflexia, it makes it easier to know what to do to prevent it.
Since an overfull bladder is the most common cause, it’s usually best to start there. If Foley/Suprapubic/Condom catheters are being used, be sure to keep the tube free of kinks and empty the collection bag frequently. Also, check inside of the tube frequently for any kind of grit or deposit that may indicate that you have an infection or a stone. This may be a sign that your Foley catheter needs to be changed or irrigated as well. If intermittent catheterization is used, be sure to do it frequently enough to keep the bladder from filling.
The best prevention when it involves bowels is to maintain a regular bowel program. Avoid constipation by eating plenty of fiber (fruits and vegetables) and drink enough water. If hemorrhoids are present, be sure to treat them.
Do pressure reliefs frequently to avoid pressure sores. Check skin carefully every day for sores or other skin problems. Avoid wearing tight or restrictive clothing. Check clothing for sharp or hard objects that can rub or cause pressure (for example, buttons on rear pants pockets).
Refrain from long exposure in the sun and use a sunscreen to prevent sunburns. In general, avoid extreme hot or cold temperatures
SILENT AUTONOMIC DYSREFLEXIA
A sign of AD is a rise of 20 to 40 in the baseline systolic blood pressure along with other symptoms discussed earlier. Current research shows that significant elevations in blood pressure can occur without signs and symptoms of AD (asymptomatic). This condition is known as “Silent” Autonomic Dysreflexia. To date, “Silent” AD has been studied during the time of urination, digital stimulation of the bowels, and ejaculation during sexuality in men with SCI. It appears that people at risk for AD are also at risk for “Silent” AD. However, it seems that people who have never reported having an episode of AD still experience “Silent” AD. “Silent” AD has shown to be common during some activities, and it may also prove to be common with other activities. Further research is now needed to determine whether or not “Silent” AD poses the same dangers as AD and preventive medications are needed. If you have concerns, talk with your doctor.
Individuals need a plan of action should they experience any signs or symptoms of AD. First, individuals should get in a seated position. Second, look for the cause and remove the irritation. If the cause is not found or symptoms continue, seek emergency treatment immediately. Anyone who has a spinal cord injury at or above the level of T-6 should:
Understand the signs, symptoms, causes and treatment of dysreflexia;
- Have equipment for taking blood pressure available and know how to use it;
- If a systolic pressure is greater than 150, it is crucial to seek emergency treatment immediately because it can result in a stroke, seizure or death.
- Keep a few tablets of Nifedipine (Procardia) on hand for emergencies (take only as prescribed).
- Keep a “Medical Alert” card with you at all times, especially when away from home.
- Be sure that all of your doctors have information about Autonomic Dysreflexia.
SEXUALITY AND REPRODUCTIVE HEALTH
Sexuality and reproductive health for men with SCI
A spinal cord injury (SCI) affects a man’s sexuality both physically and psychologically. After injury, men may face changes in relationships, sexual activity, and their ability to biologically father children. Men can also experience emotional changes that can affect sexuality. All of these issues involve both the man with SCI and his partner. Therefore, it is very important to understand and confront these issues as a part of the overall adjustment to life after injury.
Many men with SCI are capable of having an erection. However, the erection may not be hard enough or last long enough for sexual activity. This condition is called Erectile Dysfunction (ED). There are various treatments and products available for treating ED but men with SCI may have special concerns or problems with their use. It is important to see a doctor or urologist for accurate information on the various treatments and products available.
Men with SCI also experience a change in their ability to biologically father a child. The major factor interfering with a man’s fertility is primarily due to an inability to ejaculate as a result of damage to the spinal cord. In fact, 90% of men with SCI are not able to ejaculate during intercourse; this is called anejaculation. Another problem men with SCI may experience is retrograde ejaculation. This occurs when semen does not leave the urethra but travels back up the tube and is deposited in the bladder.
Options are available to assist men with spinal cord injury improve their ability to father children. Men who are interested in fathering a child should get medical advice and treatment options from a fertility specialist experienced in issues of spinal cord injury. The fertility specialist needs to be aware of methods that can improve sperm quality in men with SCI, as well as complications that can occur, such as autonomic dysreflexia.
A romantic and intimate relationship with a partner can be developed or maintained after a spinal cord injury. It is important to keep the lines of communication open as well as an openness to explore and experiment with different ways to be intimate. Together, you can discover what it takes to maintain a sexually stimulating and fulfilling relationship.
Sexuality and Reproductive Health for Women with SCI
Women with a spinal cord injury represent about 20% of all individuals with SCI/D and the majority of these women are of childbearing age. Regardless of a woman’s level of injury or dysfunction, women with SCI can engage in sexual activity, can have children and will need to use a contraceptive method if they choose not to have children. Education is the key for women with SCI/D to understand the facts related to pregnancy, labor, and delivery. The first step in the journey towards motherhood is visiting with an obstetrician. If your obstetrician has limited experience in managing pregnancies of women with SCI/D, it is recommended that you take a “team” approach to your pregnancy. You and your obstetrician can consult with an experienced physiatrist, nurse, urologist, anesthesiologist, neurologist, respiratory therapist, physical therapist, and occupational therapist on specific concerns about pregnancy, labor and delivery. Although women with SCI/D may be considered to have “high risk” pregnancies, it does not mean that pregnancy should be avoided. It simply means that you need to take precautions to prevent and treat complications. Pregnant women with SCI/D are at greater risk for developing:
- Autonomic Dysreflexia (AD)
- Changes in bowel function (constipation or diarrhea)
- Bladder spasms resulting from increased weight on the bladder
- Urinary tract infections (a UTI might actually trigger premature labor if not properly managed)
- Pressure sores resulting from weight gain and/or posture changes
- Respiratory complications
- Muscle Spasms
- Swelling of the legs and feet caused by lack of blood flow in the lower extremities
Many prescribed and over-the-counter medications normally used by women with SCI/D can cause problems during pregnancy. Some medications can also have an adverse effect on fetal growth. Therefore, it is essential that all medications be evaluated by your obstetrician before pregnancy and continually re-evaluated each trimester. Some conditions that you might manage with medications include bowel management, pain, sexual dysfunction, muscle spasms, and urinary tract infection (UTI). Some women with SCI/D may have signs of labor, while others may not. Therefore, those with SCI/D must be aware of the common signs of labor, including abdominal tightening, changes in breathing, backache. Autonomic Dysreflexia is common during labor and can be life threatening if not managed properly.
Most women can, and should, deliver vaginally whenever possible. Some may deliver with ease, while others may need the assistance of a vacuum device or forceps. Some women with SCI/D have skeletal abnormalities such as curvature of the spine, pelvic fracture, or hip dislocation. These conditions can limit the space in the abdomen necessary to carry a full-term fetus. These abnormalities can make vaginal delivery difficult. In these cases, a Caesarean section (C-section) may be necessary.
Once the baby is born, the decision on whether or not to breast-feed must be made.
Although breast-feeding is possible for most women, you may notice an increase in your spasticity as you breast-feed. Also, breast-feeding normally stimulates the production of breast milk, so women with limited sensation in their nipples may notice a reduction in milk.
Although there are risks for complications related to pregnancy, risks can be reduced and managed through proper prenatal care and adequate planning.
REHABILITATION
Individuals who have recently suffered a spinal cord injury (SCI) may experience many emotions, such as fear or anxiety. Many individuals may require spinal cord injury rehabilitation to adapt to a new way of life after the injury.
How Does Rehabilitation Help People Recover From Spinal Cord Injuries?
No two individuals will experience the same emotions after surviving a spinal cord injury, but almost everyone will feel frightened, anxious, or confused about what has happened. Individuals commonly have very mixed feelings after suffering an SCI: relief that they are still alive, but disbelief at the nature of their disabilities.
Rehabilitation programs combine physical therapies with skill-building activities and counseling to provide social and emotional support. The education and active involvement of the injured individual and his or her family and friends is critical.
A rehabilitation team is usually led by a doctor specializing in physical medicine and rehabilitation (called a physiatrist), and often includes social workers, physical and occupational therapists, recreational therapists, rehabilitation nurses, rehabilitation psychologists, vocational counselors, nutritionists, and other specialists. A case-worker or program manager coordinates care for the injured individual.
In the initial phase of rehabilitation, therapists emphasize regaining leg and arm strength since mobility and communication are the two most important areas of function. For some, mobility will only be possible with the assistance of devices such as a walker, leg braces, or a wheelchair. Communication skills, such as writing, typing and using the telephone may also require adaptive devices.
Physical therapy includes exercise programs geared toward muscle strengthening. Occupational therapy helps redevelop fine motor skills. Bladder and bowel management programs teach basic toileting routines, and patients also learn techniques for self-grooming. People acquire coping strategies for recurring episodes of spasticity, autonomic dysreflexia, and neurogenic pain.
Vocational rehabilitation begins with an assessment of basic work skills, current dexterity, and physical and cognitive capabilities to determine the likelihood for employment. A vocational rehabilitation specialist then identifies potential work places, determines the type of assistive equipment that will be needed, and helps to arrange for a user-friendly workplace. For those individuals whose disabilities prevent them from returning to the workplace, therapists focus on encouraging productivity through participation in activities that provide a sense of satisfaction and self-esteem. This could include educational classes, hobbies, memberships in special interest groups, and participation in family and community events.
Recreation therapy encourages patients to build on their abilities so that they can participate in recreational or athletic activities at their level of mobility. Engaging in recreational outlets and athletics helps those with spinal cord injuries achieve a more balanced and normal lifestyle and also provides opportunities for socialization and self-expression.