Brain Computer Interface Allows Monkey To Control Robotic Arm

Hitachi Brain Control Device To Assist Traumatic Brain & Spinal Injury Patients

Hitachi has been working on the development of a brain control device that will allow traumatic brain and spinal cord injury patients flexibility in their everyday life.The original hardware for a device that utilizes this technique was developed by Hitachi, and it allows a person with locked-in syndrome to say “yes” or “no.”
Allowing the user to forget the TV remote clicker and control electronic devices without lifting a finger simply by reading brain activity.The “brain-machine interface” developed by Hitachi Inc. analyzes slight changes in the brain’s blood flow and translates brain motion into electric signals.
A cap connects by optical fibers to a mapping device, which links, in turn, to a toy train set via a control computer and motor during one recent demonstration at Hitachi’s Advanced Research Laboratory in Hatoyama, just outside Tokyo.
A researcher, demonstrated the device by telling a reporter to take a deep breath and relax. At his prompting, a reporter did simple calculations in her head, and the train sprang forward — apparently indicating activity in the brain’s frontal cortex, which handles problem solving.
Activating that region of the brain — by doing sums or singing a song — is what makes the train run, according to the researcher. When the user stops the calculations, the train also stops. Hitachi’s scientists are set to develop a brain TV remote controller letting users turn a TV on and off or switch channels by only thinking. The technology could one day replace remote controls and keyboards and perhaps help disabled people operate electric wheelchairs, beds or artificial limbs.
Although brain-machine interface technology has traditionally focused on medical uses, makers like Hitachi and Japanese automaker Honda Motor Co. have been racing to refine the technology for commercial application. Honda, whose interface monitors the brain with an MRI machine like those used in hospitals, is keen to apply the interface to intelligent, next-generation automobiles.
Underlying Hitachi’s brain-machine interface is a technology called optical topography, which sends a small amount of infrared light through the brain’s surface to map out changes in blood flow. Initial uses would be helping people with paralyzing diseases communicate even after they have lost all control of their muscles.
Since 2005, Hitachi has sold a device based on optical topography that monitors brain activity in paralyzed patients so they can answer simple questions, for example, by doing mental calculations to indicate “yes” or thinking of nothing in particular to indicate “no.”
“We are thinking of various kinds of applications,” project leader Hideaki Koizumi said. “Locked-in patients can speak to other people by using this kind of brain machine interface.”
A key advantage to Hitachi’s technology is that sensors don’t have to physically enter the brain. Earlier technologies developed by U.S. companies like Neural Signals Inc. required implanting a chip under the skull.
Still, major stumbling blocks remain.
Size is one issue, though Hitachi has developed a prototype compact headband and mapping machine that together weigh only about two pounds. Japanese electronics giant Hitachi has unveiled a proto-type model of a portable brain-machine interface lately. This portable brain-machine interface is equipped with eight pairs of lasers and optical sensors in a special headband (weighting 400gram to 630gram) to measure prefrontal cortex activity. It senses activity from the user’s brain and converts it into signals to control electronic devices. It’s pretty cool!
In fact Hitachi demonstrated an early prototype in November last year. The device enabled users to turn on/off the power switch with a thought. It was very unique but the design of the headset was a bit old-fashioned. This latest brain-machine interface selling at US$840,000 which is shown at Hitachi’s headquarters in Tokyo represents an enormous leap forward compared to the previous version. Hitachi says the system is easy to use and that it has been built using parts from models designed for medical applications.
Another would be to tweak the interface to more accurately pick up on the correct signals while ignoring background brain activity.
Any brain-machine interface device for widespread use would be “a little further down the road,” Koizumi said.
Brain Controlled Devices Help Paralyzed People
Brian Controlled Devices will help the 6 Million Americans suffering from Traumatic Brain and/or Spinal Cord Injuries resulting in their becoming paralyzed. For those living with paralysis, mentally controlling artificial limbs and mobility devices would be a big step forward toward more independent living.
Melody Moore Jackson, director of the BrainLab at the Georgia Institute of Technology, is trying to make that happen.
Jackson started this lab in 1998 to look at methods of brain control that didn’t involve surgery. At that time, she estimates, there were about five labs working on the same topic of brain-computer interfaces. Now there are about 300.
Neutral Control For Assistive Technology
The BrainLab was one of the first to demonstrate that a person can control a robotic arm and a wheelchair with brain signals,
“We can literally influence the wiring of the brain, rewiring the brain, so to speak, to allow them to make new neural connections, and hopefully to restore movement to a paralyzed arm,” Jackson said.
A smaller subset in need of such technologies consists of patients with locked-in syndrome, a rare neurological disorder. These patients feel, think, and understand language, but cannot move or speak — they are “prisoners in their own bodies,” Jackson explained.
The Diving Bell and the Butterfly
A famous example is Jean-Dominique Bauby, who became locked-in after a stroke, and wrote the memoir “The Diving Bell and the Butterfly” by blinking to indicate individual letters. Jackson wants to open up possibilities for people with locked-in syndrome to communicate and move.
One technique that Jackson and colleagues use to harness brain signals is called functional near-infrared spectroscopy. This involves shining a light into the brain to discern how much activity is there, and examining the corresponding oxygen level.
Light at a specific wavelength is beamed into the brain, and the oxygen present will absorb some of that light. This allows scientists to pick up on small differences in the blood’s oxygenation.
For example, scientists can place a sensor over the Brocca’s area, a part of the brain essential for language. This area is activated when you talk to yourself inside your head or count silently, which is called subvocal speech.
Scientists can use the oxygen levels associated with this to create a system of allowing a person to say “yes” and “no” just by thinking; “no” corresponds to no subvocal speech or nonsense syllables.
Advancing Research on Brain Controlled Devices
But Jackson wanted to make something more interesting to learn. Her group created a hot-air balloon video game, where the balloon reflects the blood oxygenation level. Multiple locked-in syndrome patients can compete with each other in this game.
“It’s not necessarily just for fun,” Jackson said. “We can actually say, ‘Well, they got 70% of the obstacles correct, they were able to jump over the mountains or get through the wind.’ And so it also allows us to collect data.”
In the stroke rehabilitation arena, Jackson’s group hopes to restore movement in people who have paralysis or partial paralysis in a limb.
Researchers are looking at a rehabilitation robot called an exoskeleton, a device that a person sits in to be able to move limbs that they wouldn’t otherwise. The robot can detect the brain signal corresponding to a person thinking about moving an arm, and then move the arm.
“What we’re trying to do is make new neural connections from the brain to the arm,” Jackson said.
The lab has also developed a wheelchair that a person can drive by using brain signals, rather than moving a joystick or pressing buttons.
Such brain-computer interfaces require that the user wear an EEG cap to measure brain signals, but setting one up is very complicated. Jackson hopes to make it accessible for anyone to use in their own home.
“You can imagine how much faster the therapy would go if you were doing it all the time,” she said.
Paralyzed Man Who Walks After 25 Years

This is the story of John Maclean a determined paralyzed man, who walks after 25 years:
John Maclean at the age of 22, he was a reserve-grade player for the precursor to the Australian National Rugby League – the New South Wales Rugby League, as well a burgeoning triathlete.
Those dreams were thought to have been shattered on June 27, 1988, when Maclean was struck from behind by an eight-ton truck while on the road training for the upcoming Nepean Triathlon on his bicycle. The collision left Maclean with a broken back, pelvis and right arm. From that moment on, Maclean was rendered a paraplegic.
From a moment in time when some would give up and fall, Maclean picked himself up – again, and again, and again. His determination undaunted, his resolve unwavering and his competitive fire burning more intense than ever, Maclean began to train, to compete, to win.
His first stop was a return to Nepean in 1994 where he became Australia’s first paraplegic triathlete. He then became the first person in a wheelchair to complete the Ironman World Championship in Kona, and the first to swim the treacherous English Channel — not once, but twice (1995, 1998). He even trained with the national wheelchair basketball team in 1995 as they prepared for the 1996 Atlanta Olympics.
After 25 years of being in a wheelchair, John started working with Ken Ware in 2013 and on day 4 he took his first unassisted steps. Since working with Ken, John has been able to walk leaving his wheelchair behind while strolling along the beach hand in hand with his wife and pick up his son. John’s goal is to now run on the beach and compete in an Ironman.
The ultimate dream Maclean speaks of is finishing what he started — to race Nepean, Australia’s oldest continuing triathlon — out of the wheelchair and on his own two feet. With the help of Neurophysicist Ken Ware, founder of Neurotricional Sciences, whom he met through mutual friend and 2012 Ironman World Champion Pete Jacobs, Maclean is now walking.
John became a special case because of his circumstances, being a partial paraplegic, which meant some signals were able to get through and Ken was able to exploit those small pathways and create new, much larger ones relatively quickly, which meant obvious results, quickly,” he said. “There is no doubt John will complete this goal. He is an amazingly talented and strong individual, and he will keep progressing with his abilities between now and then.”
NeuroPhysics Functional Performance Training and Rehabilitation (NPTR) is a scientifically based and clinically proven method, which has broad applications across many aspects of rehabilitation and performance.
NPTR is a fully integrated, holistic program that engages all of the body’s systems in a unique way, to optimise recovery from a variety of conditions, as well as enhance physical performance and wellbeing.
NPTR is a method of activating communication in the nervous system that connects pathways in a manner that has not been previously discovered and explained. The therapy does not discriminate, as it focuses on treating the person, not the disorder, with results achieved in remarkable timescales.
NPTR is an exercise based program that utilises specific equipment and techniques to firstly assess the status and function of a client’s system, and then trigger the nervous system to self organize and return itself back to optimal function.
As stated in Frontiers In Physiology, in contrast to conventional physical therapies, this therapy involves no physical manipulation of the treated individual. Individuals perform the exercises on their own with instructive coaching support. The exercises are not tailored to particular presenting conditions: the same approach is used regardless of age, injury, medical history, or disorder. Treatment is a phased process. Session frequency during the brief initial treatment period may vary from daily, to alternating days, to several days apart, depending on the client. In the remainder of the first month, clients begin the self-administered, standardized progression of ongoing exercise programs for strengthening and maintaining physical and executive control.
Read more: The John Maclean Story: Standing Tall… | TriRadar.com http://www.triradar.com/news/the-john-maclean-story-standing-tall/#ixzz3BVpQy7jv
Traumatic Brain Stem Stroke Paralysis

Following a car crash, Mr. Constantine had a traumatic brain stem stroke that caused paralysis on the right side of his body. His leg muscles became so severely spastic that he could not walk. After four years of confinement to a wheelchair, Rick Constantine, 58, is now walking again after undergoing an unconventional surgery at University of California, San Diego Heath System to restore the use of his leg. Neurosurgeon Justin Brown, MD, director of the Neurosurgery Peripheral Nerve Program at UC San Diego Health System, performed the novel 3-hour procedure. His team performed a delicate surgery to reduce input from the nerves that were causing the muscles to over contract to the point of disability.
“After my injury, I was told I would never walk again. All I could to was move from my wheelchair to my bed or a chair,” said Constantine, a former NASCAR crew member. “After surgery with Dr. Brown, I could put my foot flat on the ground to walk. With physical therapy, everything just gets better and better. I’m a firm believer in never giving up.”
Prior to surgery, Constantine underwent botox treatments and physical therapy in an attempt to restore the use of his leg following the injury due to his traumatic brain stem stroke. The results were positive but minimal. An additional nerve conduction study, called an electromyogram (EMG), identified the muscles causing the dysfunction.
“When all other options did not produce satisfying results, we opted for surgery,” said Brown. “With the EMG, we identified the over excited nerves resulting from the traumatic brain stem stroke, which needed to be downgraded. Mr. Constantine had surgery on a Friday and within days was in physical rehabilitation. Two weeks later he was walking without a walker and has even completed a 1-mile race without assistance.”
The surgery, called a selective peripheral neurotomy, is a procedure performed under a microscope. Brown makes an incision behind the knee to reach the tibial nerve. He then selectively trims back the troublesome nerve branches by up to 80 percent. Cutting the nerve reduces the “noise” being relayed back to the spinal cord which causes the spasticity.
Brown, who also serves as co-director of the Center for Neurophysiology and Restorative Neurology at UC San Diego Health System, said the advantage to this approach is that the muscle is preserved and there is no need to cut or lengthen the tendon.
Depending on the specific patient and their medical history, selective peripheral neurotomy may be appropriate for patients with brain and spinal cord injury from strokes or tumors, cerebral palsy, or multiple sclerosis.
No special post-operative care is required as the sutures are absorb-able. Rehabilitation can begin 72 hours after the procedure and Constantine underwent physical therapy at VIP Neuro-Rehabilitation Center in San Diego.
Dr. Justin Brown has performed this surgery on six patients, which is seldom performed in the United States, but more common in France and Japan.
Published in Science Daily
Spinal Cord Rehab Breakthrough
A Spinal Cord rehab breakthrough occurred at the University of Louisville Spinal Cord research lab , when neuroscientist Susan Harkema turned her back to her study subject to check a reading on a computer screen.
“Hey Susie, look at this,” the patient called out to her. “I can move my toe!“
It’s not the first time electrical stimulation has made paralyzed patients move, but Harkema says it’s the first time electrical stimulation directly to the spinal cord has shown voluntary activity. Experts say this new technique is another piece of the puzzle toward helping paralyzed people walk again. And it’s another avenue doctors can go down to try to help these patients.
Brain-controlled devices may help paralyzed people
“This is a breakthrough,” says Dr. Barth Green, co-founder of The Miami Project to Cure Paralysis at the University of Miami, who was not involved in the research. “It shows you can have a living spinal cord under the layer of their injury.”
More than 1,700 paralyzed people have inquired about using this technology, which involves surgically implanting a stimulator and giving it directions with an external remote control. The stimulator creates a small, slightly visible bulge in the lower abdomen and is connected to wires that send electrical pulses to the spinal cord.
But patients shouldn’t expect that the stimulator will help them walk, since the stimulator can only make one leg work at a time. Patients have to turn the stimulator off and then back on again to make the other leg work or to make another set of muscles such as their torsos work.
Even though Dustin Shillcox, the fourth patient to try the device, can’t walk, the stimulator has had other benefits dramatically improving bladder, bowel and sexual function amazingly changing his entire life.
Plus, tests showed the patients, who could finally move their legs and torsos after years of paralysis, became healthier in general with improved heart and respiratory function.
“If you can change health and wellness and life expectancy, to me that’s a home run,” Green says. “Remember, Christopher Reeve died from complications of immobility,”
The researchers are pretty much stumped as to exactly why electrical stimulation to the spinal cord created the movement on demand — after all, they didn’t touch the patients’ brains. Perhaps, Harkema says, the spinal cord in a way has a brain of its own. “Maybe the spinal cord makes the decision to move on its own and then executes the movement,” Harkema says. “Otherwise I don’t know how you would see what we see today.”
The Louisville researchers now have funding to implant the device in eight more patients. They hope a device company will help them come up with a way to stimulate more than one muscle group at the time.
Traumatic Brain & Spinal Cord Injury Effects

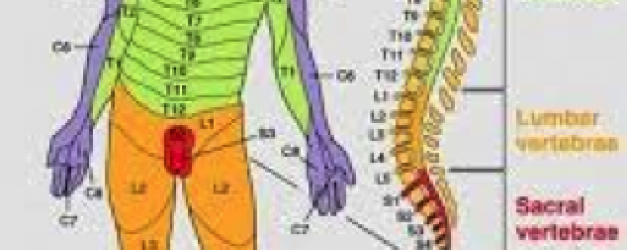
Traumatic Brain or Spinal Cord Injury can result in damaging neurons in the brain or spinal cord. When communication between the brain and spinal cord fails, paralysis occurs affecting only the areas below the level of injury.
Messages are passed from neuron to neuron through small gaps between the cells, with the help of chemicals called neurotransmitters. To transmit an action potential message neurotransmitter molecules are released from one neuron across the gap to the next neuron this process continues until the message reaches its destination.There are millions and millions of connections between neurons within the spinal cord alone which connections are made during our body’s development.
NEUROTRANSMITTERS are the brain chemicals that communicate information throughout our brain and body. They relay signals between nerve cells, called “neurons.” The brain uses neurotransmitters to tell your heart to beat, your lungs to breathe, and your stomach to digest. They can also affect mood, sleep, concentration, weight, and can cause adverse symptoms when they are out of balance. Neurotransmitter levels can be depleted many ways – from stress, poor diet, neurotoxins, genetic predisposition, drugs , alcohol and caffeine usage.
There are two kinds of neurotransmitters – INHIBITORY and EXCITATORY. Excitatory neurotransmitters are not necessarily exciting – they are what stimulate the brain. Those that calm the brain and help create balance are called inhibitory. Inhibitory neurotransmitters balance mood and are easily depleted when the excitatory neurotransmitters are overactive.
Inhibitory Neurotransmitters
SEROTONIN is an inhibitory neurotransmitter – which means that it does not stimulate the brain. Adequate amounts of serotonin are necessary for a stable mood and to balance any excessive excitatory (stimulating) neurotransmitter firing in the brain. If you use stimulant medications or caffeine in your daily regimen – it can cause a depletion of serotonin over time. Serotonin also regulates many other processes such as carbohydrate cravings, sleep cycle, pain control and appropriate digestion. Low serotonin levels are also associated with decreased immune system function.
GABA is an inhibitory neurotransmitter that is often referred to as “nature’s VALIUM-like substance”. When GABA is out of range (high or low excretion values), it is likely that an excitatory neurotransmitter is firing too often in the brain. GABA will be sent out to attempt to balance this stimulating over-firing.
DOPAMINE is a special neurotransmitter because it is considered to be both excitatory and inhibitory. Dopamine helps with depression as well as focus, which you will read about in the excitatory section.
Excitatory Neurotransmitters
DOPAMINE is our main focus neurotransmitter. When dopamine is either elevated or low – we can have focus issues such as not remembering where we put our keys, forgetting what a paragraph said when we just finished reading it or simply daydreaming and not being able to stay on task. Dopamine is also responsible for our drive or desire to get things done – or motivation. Stimulants such as medications for ADD/ADHD and caffeine cause dopamine to be pushed into the synapse so that focus is improved. Unfortunately, stimulating dopamine consistently can cause a depletion of dopamine over time.
NOR-EPINEPHRINE is an excitatory neurotransmitter that is responsible for our stimulation processes in the body. Norepinephrine helps to make epinephrine as well. This neurotransmitter can cause ANXIETY at elevated excretion levels as well as some “MOOD DAMPENING” effects. Low levels of norepinephrine are associated with LOW ENERGY, DECREASED FOCUS ability and sleep cycle problems.
EPINEPHRINE is an excitatory neurotransmitter that is reflective of stress. This neurotransmitter will often be elevated when ADHD like symptoms are present. Long term STRESS or INSOMNIA can cause epinephrine levels to be depleted (low). Epinephrine also regulates HEART RATE and BLOOD PRESSURE.
Optical Brain Scanner Future for Traumatic Brain Injuries

This new development utilizing an Optical Brain Scanner may revolutionize the future treatment of Traumatic Brain Injury patients due to its portability and non-invasive technology. With further refinement and development, these features will allow EMT’s to do a comprehensive evaluation on the patient prior to transporting them to the hospital and share the imaging data with neurologists.
Scientists have advanced a brain-scanning technology that tracks what the brain is doing by shining dozens of tiny LED lights on the head. This new generation of neuroimaging compares favorably to other approaches but avoids the radiation exposure and bulky magnets the others require, according to new research at Washington University School of Medicine in St. Louis.
The new optical approach to brain scanning is ideally suited for children and for patients with electronic implants, such as pacemakers, cochlear implants and deep brain simulators (used to treat Parkinson’s disease). The magnetic fields in magnetic resonance imaging (MRI) often disrupt either the function or safety of implanted electrical devices, whereas there is no interference with the optical technique.
The new technology is called diffuse optical tomography (DOT). While researchers have been developing it for more than 10 years, the method had been limited to small regions of the brain. The new DOT instrument covers two-thirds of the head and for the first time can image brain processes taking place in multiple regions and brain networks such as those involved in language processing and self-reflection (daydreaming).
The results are now available online in Nature Photonics.
“When the neuronal activity of a region in the brain increases, highly oxygenated blood flows to the parts of the brain doing more work, and we can detect that,” said senior author Joseph Culver, PhD, associate professor of radiology. “It’s roughly akin to spotting the rush of blood to someone’s cheeks when they blush.”
The technique works by detecting light transmitted through the head and capturing the dynamic changes in color of the brain tissue.
Although DOT technology now is used in research settings, it has the potential to be helpful in many medical scenarios as a surrogate for functional MRI, the most commonly used imaging method for mapping human brain function. Functional MRI also tracks activity in the brain via changes in blood flow. In addition to greatly adding to our understanding of the human brain, fMRI is used to diagnose and monitor brain disease and therapy.
Another commonly used method for mapping brain function is positron emission tomography (PET), which involves radiation exposure. Because DOT technology does not use radiation, multiple scans performed over time could be used to monitor the progress of patients treated for brain injuries, developmental disorders such as autism, neurodegenerative disorders such as Parkinson’s, and other diseases.
Unlike fMRI and PET, DOT technology is designed to be portable, so it could be used at a patient’s beside, in the operating room.or at point of injury as in the case of Traumatic Brain Injuries and concussions.
“With the new improvements in image quality, DOT is moving significantly closer to the resolution and positional accuracy of fMRI,” said first author Adam T. Eggebrecht, PhD, a postdoctoral research fellow. “That means DOT can be used as a stronger surrogate in situations where fMRI cannot be used.”
For the current study, the researchers validated the performance of DOT by comparing its results to fMRI scans. Data was collected using the same subjects, and the DOT and fMRI images were aligned. They looked for Broca’s area, a key area of the frontal lobe used for language and speech production. The overlap between the brain region identified as Broca’s area by DOT data and by fMRI scans was about 75 percent.
“With the improved image quality of the new DOT system, we are getting much closer to the accuracy of fMRI,” Culver said. “We’ve achieved a level of detail that, going forward, could make optical neuroimaging much more useful in research and the clinic.”
While DOT doesn’t let scientists peer very deeply into the brain, researchers can get reliable data to a depth of about one centimeter of tissue. That centimeter contains some of the brain’s most important and interesting areas with many higher brain functions, such as memory, language and self-awareness represented.
During DOT scans, the subject wears a cap composed of many light sources and sensors connected to cables. The full-scale DOT unit takes up an area slightly larger than an old-fashioned phone booth, but Culver and his colleagues have built versions of the scanner mounted on wheeled carts. They continue to work to make the technology more portable.
The research is funded by the National Institutes of Health (NIH) grants R01-EB009233, R01-NS078223, T32-NS007205-30 and P30-NS048056; an Autism Speaks Postdoctoral Translational Research Fellowship; a Fulbright Science and Technology PhD Award; and a McDonnell Centre for Systems Neuroscience grant.
Traumatic Brain Injury and Spinal Cord Patients can Develop Ease of Living Space
Traumatic Brain Injury and Spinal Cord patients require several unique adaptations to revamping their everyday living environment to facilitate the disabilities they have experienced. One of the several obstacles they face is how to undertake a redesign of their existing space economically while making the home capable of accommodating their needs.
Dave Ward, a quadriplegic at age 30, redesigned his 1855 Historic Home to fit his needs and estimates that today it would cost approximately $9,000 to replicate the revisions he made. Following is an interview he gave to NPR in text format and a link to the audio version.
http://www.npr.org/player/v2/mediaPlayer.html?action=1&t=1&islist=false&id=6303285&m=6303290
“Dave Ward is the resident curator of the place he calls the Future Home, a house that he has turned into a model of “universal design.” It’s the idea that where we live — and the technology and products we use — should be designed so they are easy to use for anybody, including a quadriplegic, like Ward or an elderly person who’s frail or has cognitive disabilities.”
The Future Home is in the middle of a state park in Phoenix, Md., about an hour north of Baltimore. The house is historic, but it mixes the old with the futuristic.
“This house was first built in 1855,” Ward explains, “It was built as a tavern and inn, and it served the horse and buggy trade that traveled from Baltimore to Harrisburg, Pa.”
Back then, this big, white building was known as Smith’s Tavern. It’s right up against the old toll road. Today, on the long wraparound porch, the music of the wind chimes competes with the noise of the cars rushing by.
“Horse and buggies didn’t make as much noise as cars do,” Ward says.
Ward became interested in universal design by necessity. In 1977, at the age of 30, he became a quadriplegic after a fall.
Ward lived in this house before his accident. Now he has redesigned it so his personal-care attendant can live upstairs. The downstairs, where Ward lives, is a showcase of universal design, built to allow him to live as independently as possible. But he’s also made it a model for other disabled people as well as the elderly. Architects, designers and consumers come from around the world to see Ward’s house.
He starts the tour outside, at the main entrance.
“If we’re talking about access or universal design or home modifications, it all starts outside,” says Ward. “One of the things that’s real important for people is a place to park their automobile, and then to get from that mode of transportation to the front door without any barriers. In most cases, those barriers end up being steps.”
When Ward redesigned this place, he moved the main entrance to the back of the house, removed the stairs and added a smooth path that leads from his parking spot to the door.
The entrance uses a number pad instead of a lock-and-key system. With the pointer that he keeps attached to his hand, Ward can punch in a security code and the automatic door swings open.
Ward’s personal attendant pushes his wheelchair into the kitchen. From a remote control on his wheelchair, Ward pushes a button to turn on the lights.
“The kitchen is built so it has multiple-level work surfaces,” he notes.
Varied surface levels allow people to work standing or sitting.
“Many people can’t stand long enough to do an entire task,” he says. “For example, cooking or washing dishes or cleaning vegetables. And they want to sit.”
So there are two sinks on the blue and pink kitchen island in the middle of the large, square room. One sink is at standing height. The other is a few inches lower, for sitting. The stove top, too, can be raised or lowered to just three feet off the ground. And the cabinet of dishes comes down like an elevator.
A lot of things in Future Home move at the touch of a button. Curtains can be opened and shut by pushing a button, and a long coffee table can be raised until it becomes the dining room table.
Ward says the technology already exists to do all of this. It’s just that people don’t think of putting it in a house.
“Well, think about your car,” he says. “You’ve got climate controls all over your vehicle. We have voice control over many of the things in the car itself. We have powered windows within the car. We seem to find a way to cram that into a little vehicle, yet we haven’t looked at our own homes to think about how important it is to have the same thing there.”
Ward works in his home office as a consultant on design and on various state disability commissions.
“My favorite part of the house is probably the study,” he says. “Everything I want is within my reach in this part of the room.”
His computer is programmed to respond to his voice commands. By speaking, he can control his environment.
“Listen to me,” he commands; the computer turns on.
“Main Menu,” he says, and the computer talks back: “Okey Doke,” says the synthesized voice. Then Ward can give commands to close the shades or turn on the fan. For the television, all of the controls that you’d find on a regular TV remote control appear on his computer screen.
What would his life be like if he didn’t have a house full of all this technology?
“Well, I can tell you, because I lived it for quite a while,” he explains. “Coming home from a rehab facility, moving back into Mom’s house, it was, ‘Mom, can you take me outside? Mom, can you bring me in? Mom, can you turn the fan on? … On and on and on. Can you imagine what kind of pressure that is on an individual and how simple the technology is that we were using today to do all the things that Mom used to do for me?”
The devices add to the cost of a house, but Ward says it’s not as much as you might think, especially as more companies make more of these devices. Ward says when he built the house 14 years ago, it cost about $46,000 to put in all these devices. He says the same systems could be installed today for just a fraction of that — for less than $9,000.
Brain Implant Research To Restore Active Memory
A brain implant device that can be surgically installed in the patient’s brain to assist in forming, storing and recalling memories.
DARPA has selected two universities to initially lead the agency’s Restoring Active Memory (RAM) program, which aims to develop and test wireless, implantable “neuroprosthetics” that can help service members, veterans, and others overcome memory deficits incurred as a result of Traumatic Brain Injury (TBI) or disease. Teams will develop and test implantable therapeutic devices for memory restoration in patients with memory deficits caused by disease or trauma.
The University of California, Los Angeles (UCLA), and the University of Pennsylvania (Penn) will each head a multidisciplinary team to develop and test electronic interfaces that can sense memory deficits caused by injury and attempt to restore normal function. Under the terms of separate cooperative agreements with DARPA, UCLA will receive up to $15 million and Penn will receive up to $22.5 million over four years, with full funding contingent on the performer teams successfully meeting a series of technical milestones. DARPA also has a cooperative agreement worth up to $2.5 million in place with Lawrence Livermore National Laboratory to develop an implantable neural device for the UCLA-led effort.
“The start of the Restoring Active Memory program marks an exciting opportunity to reveal many new aspects of human memory and learn about the brain in ways that were never before possible,” said DARPA Program Manager Justin Sanchez. “Anyone who has witnessed the effects of memory loss in another person knows its toll and how few options are available to treat it. We’re going to apply the knowledge and understanding gained in RAM to develop new options for treatment through technology.”
TBI is a serious cause of disability in the United States. Diagnosed in more than 270,000 military service members since 2000 and affecting an estimated 1.7 million U.S. civilians each year, TBI frequently results in an impaired ability to retrieve memories formed prior to injury and a reduced capacity to form or retain new memories following injury. Despite the scale of the problem, no effective therapies currently exist to mitigate the long-term consequences of TBI on memory. Through the RAM program, DARPA seeks to accelerate the development of technology needed to address this public health challenge and help service members and others overcome memory deficits by developing new neuroprosthetics to bridge gaps in the injured brain.
“We owe it to our service members to accelerate research that can minimize the long-term impacts of their injuries,” Sanchez said. “Despite increasingly aggressive prevention efforts, traumatic brain injury remains a serious problem in military and civilian sectors. Through the Restoring Active Memory program, DARPA aims to better understand the underlying neurological basis of memory loss and speed the development of innovative therapies.”
Specifically, RAM performers aim to develop and test wireless, fully implantable neural-interface medical devices that can serve as “neuroprosthetics”—technology that can effectively bridge the gaps that interfere with an individual’s ability to encode new memories or retrieve old ones.
To start, DARPA will support the development of multi-scale computational models with high spatial and temporal resolution that describe how neurons code declarative memories—those well-defined parcels of knowledge that can be consciously recalled and described in words, such as events, times, and places. Researchers will also explore new methods for analysis and decoding of neural signals to understand how targeted stimulation might be applied to help the brain reestablish an ability to encode new memories following brain injury. “Encoding” refers to the process by which newly learned information is attended to and processed by the brain when first encountered.
Building on this foundational work, researchers will attempt to integrate the computational models developed under RAM into new, implantable, closed-loop systems able to deliver targeted neural stimulation that may ultimately help restore memory function. These studies will involve volunteers living with deficits in the encoding and/or retrieval of declarative memories and/or volunteers undergoing neurosurgery for other neurological conditions.
Unique to the UCLA team’s approach is a focus on the portion of the brain known as the entorhinal area. UCLA researchers previously demonstrated that human memory could be facilitated by stimulating that region, which is known to be involved in learning and memory. Considered the entrance to the hippo-campus, which helps form and store memories, the entorhinal area plays a crucial role in transforming daily experience into lasting memories. Data collected during the first year of the project from patients already implanted with brain electrodes as part of their treatment for epilepsy will be used to develop a computational model of the hippocampal-entorhinal system that can then be used to test memory restoration in patients.
After developing an advanced, new wireless neuromodulation device, featuring ten-times smaller size and much higher spatial resolution than existing devices,the UCLA team will implant such devices into the entorhinal area and hippo-campus of patients with traumatic brain injury.
The Penn team’s approach is based on an understanding that memory is the result of complex interactions among widespread brain regions. Researchers will study neurosurgical patients who have electrodes implanted in multiple areas of their brains for the treatment of various neurological conditions. By recording neural activity from these electrodes as patients play computer-based memory games, the researchers will measure “bio-markers” of successful memory function—patterns of activity that accompany the successful formation of new memories and the successful retrieval of old ones. Researchers could then use those models and a novel neural stimulation and monitoring system, being developed in partnership with Medtronic, to restore brain memory function. The investigational system will simultaneously monitor and stimulate a number of brain sites, which may lead to better understandings of the brain and how brain stimulation therapy can potentially restore normal brain function following injury or the onset of neuropsychological illness.
In addition to human clinical efforts, RAM will support animal studies to advance the state-of-the-art of quantitative models that account for the encoding and retrieval of complex memories and memory attributes, including their hierarchical associations with one another. This work will also seek to identify any characteristic neural and behavioral correlates of memories facilitated by therapeutic devices.
The performer teams are each composed of multiple universities, government research institutions, and private companies. The breadth of participation highlights the enthusiasm around the RAM program and hopes for its success.
RAM is part of a broader portfolio of programs within DARPA that support President Obama’s brain initiative. RAM’s emphasis on new discovery at a systems level reflects the great potential that lies at the heart of the president’s challenge to the neuroscience community.
RAM and related DARPA neuroscience efforts are informed by members of an independent ethical, legal, and social implications (ELSI) panel. Communications with ELSI panelists supplement the oversight provided by institutional review boards that govern human clinical studies and animal use.